This child has bilateral neuroretinitis, previously most would use the term Leber's idiopathic stellate neuroretinitis. Recently, Bartonella Henselae has been identified as the organism causing this type of neuroretinitis. It is also called Cat Scratch Disease. It is much more common than previously thought. It is a self limited disease process which commonly cause headache, loss of vision and raised intracranial pressure. Treatment often not necessary and majority recover their vision in 6-8 weeks. Children with significant encephlitis may require antibiotics treatment such as doxycycline,or erythromycin.
We ophthalmologist have a pivitol role to ascertain the diagnosis to avoid unneccessary investigation and treatments. We should also share our experience with our paediatrician colleagues, so they are aware of such common diseases.
I will attach some paragraphy of my published paper on this child and the discussion about cat scratch disease associated neuroretinitis. I hope it will be useful.
Further History about this child:
K.R.’s family has 2 cats and 3 kittens
She had close contact the cats and kittens prior to her illness
No recall of being scratched by cat, or kittens
Diagnosis ?
Serum Bartonella Henselae titre( IgG 1024) highly positive.
Bilateral Neuroretinitis associated with Cat Scratch Disease
Treatment ?
Discharge & discontinued all medications
Ophthalmology R/V 4 weeks later AKH
6 weeks later
Systemically well
VA: OD 6/9; OS 6/12+
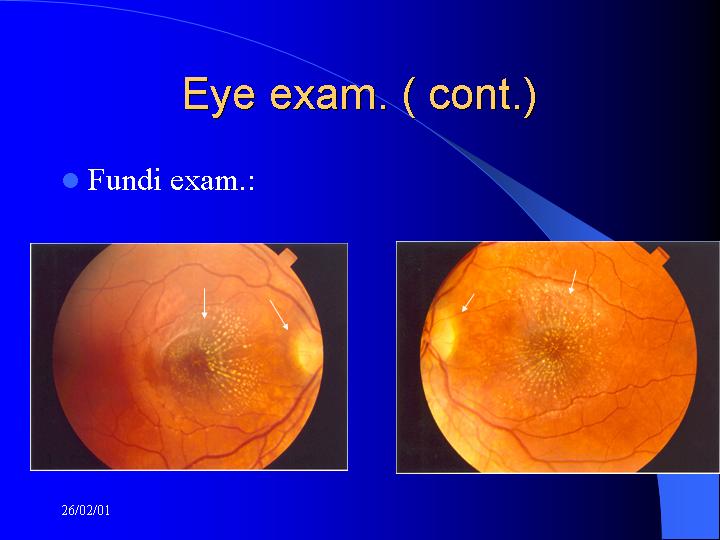
Fundi exam.:
Any changes in the discs & macula ?
Discussion
Leber’s Idiopathic Stellate Neuroretinitis. 1916.
Unilateral
Stellate macular exudates
Unknown etiology
Spontaneous resolution
Dreyer et al 1984; modified the terminology of LISN, suggesting a heterogeneous group of conditions can cause similar clinical pictures. He also pointed out that it can be bilateral.many of Leber’s cases may indeed caused by CSD.
Discussion ( cont.)
Secondary causes of Neuroretinitis:
Viral:hepatitis B,HSV,HZV,EBV influenza
Bacterial:Bartonella(CSD),TB,Syphilis,lyme disease
Fungi:histoplasmosis
Parasites & protozoa: toxoplasmosis
Others: sarcoidosis, Behcets disease
Most common:
Cat scratch disease
Toxoplasmosis
Syphilis
Lyme disease
Neuroretinitis & CSD
Wear et al. 1983, indicated the causative agent of CSD being Gram –ve Bacilli
Sweeney and Drance.1990 first described Neuroretinitis caused by CSD
Regenry et al. 1992, found high antibody titres (>1:64) to Bartonella henselae in 36 of 41 patients with CSD
Serologic evidence of CSD in Neuroretinitis 64.3% (Eric Suhler, Ophthalmology vol 107,No5 2000)
Ocular manifestations of CSD
Parinaud’s oculoglandular syndrome
Fever
Granulomatous conjunctivitis
Regional lymphadenopathy
Neuroretinitis
Loss of vision. 6/9 to PL
Disc swelling
Macular star
Focal infarct
Often unilateral, but can be bilateral
Ocular manifestations of CSD
Optic neuritis/papillitis
Uveitic syndromes
Vitritis
Acute multifocal inner retinitis,or retinal white dot syndrome
Retinitis
Choroiditis
Ocular manifestations of CSD
Retinovascular syndromes
BRVO,BRAO
Retinal vasculitis
Peripapillary angiomatosis
Others. Vf defects, ocular motor palsy
Ocular features of AIDS-associated CSD
Bacillary angiomatosis in conj & retina
Pathogenesis & Pathology
Pathogen: B. henselae
Pathogenesis still unclear, but both neural and retinal tissues are involved.retinal findings
Hx. NFL infarcts. Macular star
ONH is the principal target in acute neuroretintis, leakage on FFA
Necrotizing granulomatous lymphadenitis present
Diagnosis
High index of suspicion
Clinical features
Age. Children & adolescents account for majority cases
Systemic.regional lymphadenopathy.skin lesion
Ocular.macular star,disc swelling
Serological IFA(indirect fluorescein assay) of B. henselae
ELISAs (enzyme linked immunoassays)
IgG & IgM: cut off value > 900 (IgG) ;>250(IgM). F T Kerkhoff, BJO 1999;83:270-275
Lab variation exists.
Differentials of Macular star
Vascular : AION,BRVO,CRVO,diabetic maculopathy,HT
Papilloedema
Optic nerve head tumor or infiltrate
LISN
Treatment
Patient education and observation
Patient generally well
Spontaneous recovery of vision in most of patients
No evidence of visual recovery from proposed antibiotics Rx.
Side effects from the drugs.
Treatment
Antibiotics: doxcycline,rifampin,erythromycin,ciprofloxacin, promote resolution of CSD neuroretinitis. Lack of controlled trial.
Clear evidence of benefit from Rx in immunocompromised host.
|