Classification
- Orthophoria: The eyes are perfectly aligned, and no deviation occurs, even when the
fusion reflex is disrupted.
- Heterophoria and Heterotropia: Misalignment compensated for by the fusion reflex keeps the deviation
in heterophoria latent. Manifest misalignment is heterotropia.
- Horizontal
- Esophoria or esotropia: convergent deviation of the visual axes
- Exophoria or exotropia: divergent deviation of the visual axes
- Esophoria or esotropia: convergent deviation of the visual axes
- Vertical
- Right hyperphoria or hypertropia: right visual axis is deviated upward
compared to the left
- Left hyperphoria or hypertropia: left visual axis is deviated upward compared
to the right
- Right hyperphoria or hypertropia: right visual axis is deviated upward
compared to the left
- Torsional
- Incyclophoria or incyclotropia: superior poles of the corneas are tipped
medially
- Excyclophoria or excyclotropia: superior poles of the corneas are tipped
temporally
- Incyclophoria or incyclotropia: superior poles of the corneas are tipped
medially
- Horizontal
Determination
The methods used to determine the eye alignment in the primary position are varied and multiple. No single test invariably assesses the alignment accurately in all patients.
There are four basic types of alignment tests: the various cover tests, which depend on the fixation reflex; the corneal reflex tests, which are based on the ability of the curved corneal surface to reflect an examining light; the dissimilar image tests, which are based on the patient's response to diplopia produced by converting an isolated object of regard into different images on each retina; and the dissimilar target tests, which are based on the patient's response to the dissimilar images created by each eye viewing a different target.
COVER TESTS
Because the cover tests are based on the fixation ability of the eye, fixation ability must first be assessed. Patients without fixation ability in each eye (eccentric fixation) are unable to have eye alignment checked by cover tests. Also, the patient's accommodation must be controlled with an appropriate target. An accommodative target is a small target designed to control the patient's accommodation if the patient's response supplies clear vision; this target is required during the cover test. Advantages of cover testing include a high degree of interobserver repeatability, easy quantification using prisms, and the ability to accurately measure the angle of deviation in all fields of gaze.
Cover–Uncover.
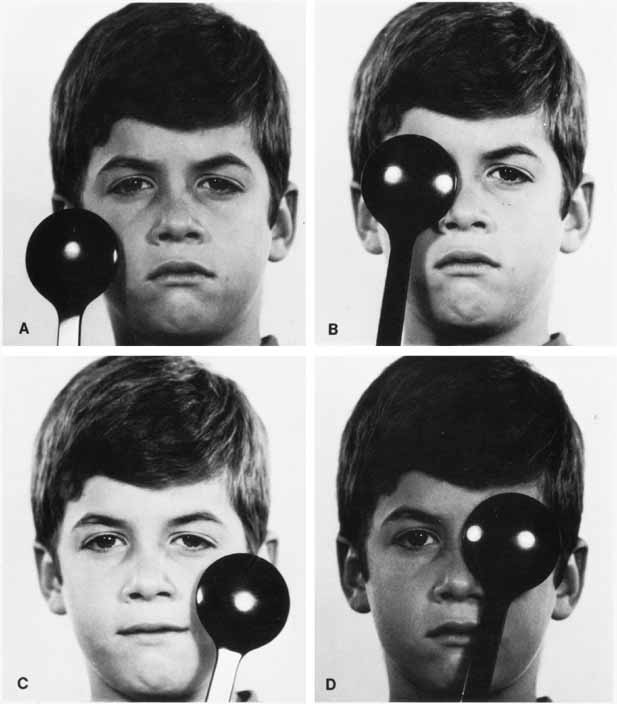
The patient's right eye is covered while fixating a series of distant accommodative targets. After 2 to 3seconds, the right eye is uncovered and the left eye covered. When covering one eye, the examiner's attention is directed to the opposite, uncovered eye, looking for movement of this eye. An absence of movement of an eye when the other eye is covered (Fig. 1), occurring in both eyes, means that the patient does not have a heterotropia, but it does not differentiate between orthophoria and heterophoria. The alternate cover test is required to make this differentiation.
Alternate Cover.
The basic principle of this test is to prevent fusion for the duration of the test. This is accomplished by constantly maintaining a cover over one or the other eye, shifting it swiftly from eye to eye while the examiner looks for movement of the uncovered eye as it assumes fixation (Fig. 2). The rapid shift applies only to the speed of movement of the cover and not to the duration it is held before the eye; in fact, the exam-iner should maintain the cover over each eye for 2 or 3 seconds before rapidly shifting it. No movement of either eye indicates orthophoria. The patient whose eye moves on alternate cover has either a heterophoria or heterotropia. Differentiation between the two requires the cover–uncover test because there is not movement for either cover–uncover or alternate cover testing in orthophoria. The direction of the shift identifies the type of heterophoria or heterotropia. A temporal horizontal shift is esophoria or esotropia, a nasal shift is exophoria or exotropia, and right or left hyperphoria or hypertropia is the movement of the right or the left eye downward. If both eyes make movements downward, it is called dissociated vertical deviation or hypertropia (see Index).
Having identified a heterodeviation, the next step is to measure the quantity of misalignment by neutralizing the shift with prism power. The prism is held in the examiner's left hand in front of the patient's right eye. The examiner's right hand handles the alternate cover. The prism or prism powers are adjusted until the motion of the eyes on alternate cover is eliminated (Fig. 2C). Base-out prisms are used to compensate for an esodeviation, base-in for an exodeviation, base-down before the right eye for a right hyperdeviation, and base-up for a left hyperdeviation. Horizontal and vertical prism powers can be combined if loose prisms are used. A prism bar is handy, but it does not lend itself to neutralizing combined horizontal and vertical deviations nor is it sufficient to compensate for horizontal deviations greater than 45Δ or vertical deviations greater than 25Δ. The loose prisms must be combined for larger deviations. Vertical deviations seldom exceed 25Δ, but horizontal tropias greater than 40Δ are very common. The most convenient way for the examiner to hold combined horizontal prisms is not to superimpose them before one eye but instead to grasp the horizontal prisms either apex-to-apex (esotropia) or base-to-base (exotropia) between the thumb and index finger of the left hand, allowing the finger and thumb to cup around the patient's right eye, with one prism being positioned before each eye. The area of contact between the apexes or bases then is in the midline in front of the patient's nose. Prisms cannot neutralize cyclodeviations.
Prism measurement of the strabismic angle is the most accurate technique for measurement. However, prism measurements are subject to error. Thompson and Guyton1 describe several potential sources of error. The angle at which the prism is held in front of the patient can influence the quantification of a deviation, especially with large angles. Two commonly used positions are the Prentice, in which the prism is held perpendicular to the line of sight of the nonfixating eye, and the frontal plane position, in which the prism is held parallel to the plane of the patient's face. In addition, the position of minimum deviation is reached when the angle of light incident to a prism is the same as that exiting. Glass prisms, although less common in clinical practice, are calibrated for the Prentice position, as are some prism bars2, whereas plastic prisms are calibrated for the angle of minimum deviation. It can be difficult to measure the angle of incident and exiting light from a prism, but in practice, the frontal plane position differs little from the angle of minimum deviation. However, holding a prism calibrated for the Prentice position in the position of minimum deviation can result in a significant overestimation of the deviation, especially for larger angles.
Strabismic angles larger than 50 prism diopters present another problem. It may be tempting to stack two prisms on top of one another and use their combined total to quantify the angle. However, this can seriously bias the result because the stacked prisms will not be held in the angle to which they are calibrated.1 Also, placing prisms in front of each other will not be correct, because angles measured in prism diopters are not additive. Fortunately, it is possible to stack horizontal and vertical prisms for complex strabismus, as the vectors are perpendicular to one another. Measurements at near are similarly subject to error.3 Because prism diopters are calculated as the distance light is bent over a distance of 1 meter, shortening the distance to a target by holding it too far from the eye can result in an overestimation of the true angle of deviation. More prism power is required to neutralize a near deviation if the prism is held several centimeters from the cornea.
Simultaneous Prism and Cover.
This test is useful in a patient having a small-angle heterotropia, commonly encountered in esotropes. The simultaneous prism and cover test is an attempt to measure the actual heterotropia angle present under normal seeing conditions while both eyes are uncovered. As the fixating eye is covered, a prism of known power is slipped simultaneously before the opposite eye with its base in the appropriate direction to compensate for the heterotropia. No movement occurs as the eye behind the prism takes up fixation when the prism power selected equals the heterotropia angle. This measurement is important because of a prevalent condition known as the monofixation syndrome.4 Some patients who have this syndrome are small-angle heterotropes; among these are some who reduce their larger fusion-free angle (as determined by alternate cover) to a smaller angle during normal seeing conditions. For example, the esotropia may measure 14Δ by alternate cover, but the simultaneous prism and cover may reveal 4Δ esotropia that the patient maintains with both eyes open.
CORNEAL REFLEX TESTS.
Studying the reflection of an examining light provides information regarding the alignment of the eyes in patients who cannot cooperate sufficiently to perform the alternate cover test or who lack fixation ability due to amblyopia. Four techniques may be employed using this principle. The Hirschberg test grossly estimates the angle of strabismus according to the degree of displacement away from the pupillary center at which the examiner views the corneal reflection in the deviated eye. Initially described by Hirschberg in the 19th century using a candle flame,5,6 currently a bright fixation light is placed before the eyes of the patient. The examiner observes the position of the light reflex in the nonfixating eye, as compared with the fixating eye. A second method was introduced by Krimsky7 as a more rigorous method of quantifying a deviated corneal light reflex. The Krimsky test entails introducing prisms before either one or both eyes to center the corneal reflections in the pupil of each eye. The third is a perimeter method, and the fourth is a major amblyoscope method. In the latter two methods, the alignment is read on the machine at the point the corneal reflections are centered in the pupils. The unit of strabismic deviation according to the Hirschberg and perimeter tests is degrees; for the Krimsky and major amblyoscope tests it is prism diopters.
Hirschberg Method.
A light reflected in the deviated eye nearer the pupillary center than the margin is estimated to be a 5° to 6° deviation, at the pupillary margin it is 12° to 15°, midway between pupillary margin and limbus it is 25°, at the limbus it is 45° to 60°, and beyond the limbus it is 60° to 80° (Fig. 3). Traditionally, each 1-mm deviation of light reflex displacement away from the proper position was considered to represent 7° or 15 prism diopters, without empirical validation.8 However, using flash photographs with millimeter rulers included for standardization, Brodie6 estimated a Hirschberg ratio of 21 prism diopters/mm, then supported this number theoretically. This angle correlates highly with that derived from alternate prism and cover testing.9
Krimsky Method.
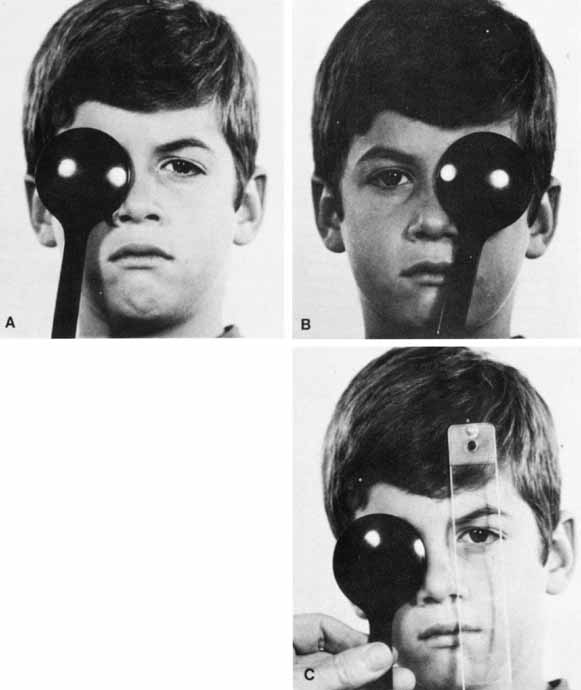
The corneal reflections of the examining light are compared in regard to the location of the pupil in each eye. Dissimilar positions are indicative of strabismus. By placing proper prism power before either one or both eyes simultaneously, the reflection can be similarly positioned (Fig. 4); this is a direct reading of the estimated squint angle. Because observation of the corneal light reflex through a prism may be difficult, von Noorden10 recommends placing the prism over the fixating eye. The Krimsky test is especially useful in younger patients, as well as patients who are unable to maintain concentration for prolonged prism and alternate cover testing and for patients with diminished central fixation in one or both eyes.
|
Both the Hirschberg and Krimsky tests have substantial limitations, the most significant of which is lack of interobserver consistency. A study11 comparing estimates of strabismic angle among 16 very experienced strabismologists found wide variability, especially using the Hirschberg method for larger angles, whereas underestimates were commonly produced. In general, the Krimsky test was more accurate than the Hirschberg test, although it was accurate less than 50% of the time. Another study12 found significant underestimation of the strabismic angle using the Krimsky method, but the amount of underestimation varied with the observer.
Perimeter Method.
The perimeter method requires the patient to steadily fixate the zero mark on the perimeter with the preferred eye while the examiner moves an examining light and his aligning eye together along the back side of the perimeter arc. At the point on the arc where the corneal reflection of the light appears located in the pupillary center of the deviated eye, the perimeter arc marking measures the squint angle in degrees (Fig. 5).
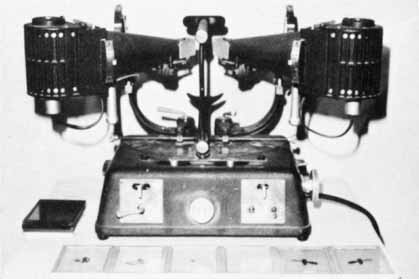
Major Amblyoscope Method.
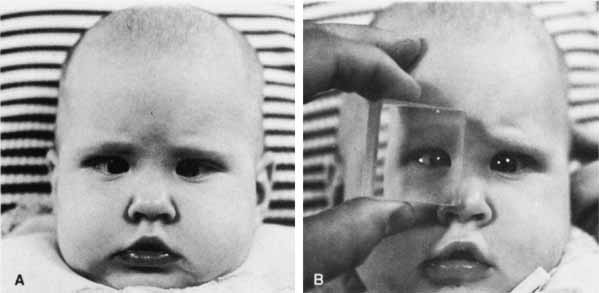
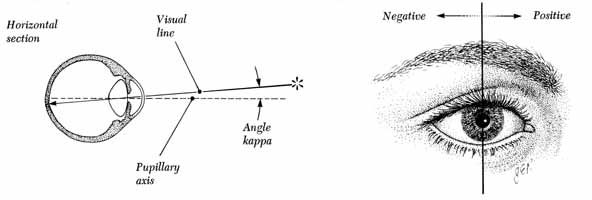
The amblyoscope is basically a refined haploscopic device that originally consisted of a median septum between the two eyes plus angled mirrors that reflected separate targets into each eye. The present-day amblyoscope, instead of using a septum and mirrors, has a separate tube for each eye with a housing at the distal end of each tube in which it is possible to insert an assortment of targets to be observed individually by each eye. Further refinements, such as separate illumination of each target that is capable of being varied by rheostats and tubes that are mounted so they can be deflected in any plane and the quantity of deflection read directly from calibrated scales, make this instrument a major amblyoscope. Adjusting the tubes so that the corneal reflections of the illumination within the target housing is centered in each pupil (Fig. 6) gives the examiner a direct reading of the patient's misalignment from the instrument's scales. Regardless of which corneal reflex technique is used, consideration must be given to the angle kappa. Because the fixation axis of the eye is not usually the exact center of the pupil, the corneal light reflex is not centered and is usually slightly nasal to the center of the pupil.3 The angle formed by an imaginary perpendicular line through the true pupillary center and the fixation axis is the angle kappa (Fig. 7). A nasal angle kappa is designated as positive and a temporal angle as negative. It can be measured by any one of the preceding methods. Corneal light reflex testing will demonstrate only the manifest portion of the deviation. Because fusion is not disrupted, the phoria component will be hidden. A situation in which a grossly positive angle kappa may be encountered is with the retinal dragging associated with retinopathy of prematurity. Because the macula may be displaced temporally, the fixation axis of the eye may be displaced even more from the papillary axis, creating a pseudoexotropia.
Both horizontal and vertical misalignments can be studied by the corneal reflex methods, but the examiner is unable to use these methods in the study of the cyclodeviations.
DISSIMILAR IMAGES TESTS.
The same fixation target, which is simultaneously presented to each eye, is converted into dissimilar images on the right and the left retina for the purpose of making fusion difficult or impossible. The Maddox rod test and the red glass test are two commonly used testing methods based on making the one object of regard project as dissimilar retinal images. Both tests are of value in assessing alignment only if the status of the retinal correspondence is known.
Maddox Rod.
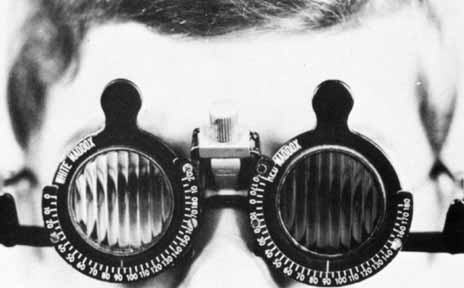
The Maddox rod is a ribbed lens, the “washboard” appearance of which converts a spot of light into a streak. The streak is seen by the patient 90° away from the axes of the multiple cylinders. The rod is placed before one eye as the other eye continues to fixate the small spot source of light; a streak is seen to pass through the light if there is no deviation in the plane being tested. A horizontal streak (ribbing of the Maddox rod is vertical) checks vertical plane alignment (Fig. 8), and a vertical streak (ribbing of the Maddox rod is horizontal) checks the horizontal plane alignment. If the streak appears displaced away from the light, a misalignment exists. Whether the misalignment is a phoria or a tropia cannot be determined because fusion is precluded in this test. In the horizontal plane testing, a homonymous diplopia indicates esodeviation, and heteronymous diplopia indicates exodeviation. In the vertical plane testing, the streak seen by the hyperdeviated eye appears lower than the light and vice versa for the hypodeviated eye. Prisms are used to eliminate the horizontal or vertical diplopia, yielding a direct measure of the deviation if the retinal correspondence is normal. Cyclodeviations can be checked by placing a Maddox rod, preferably one red and the other white, before each eye at the same axis setting for each eye. If the axes of the two Maddox rods are set at 90 (Fig. 9), the red and white streaks appear on different axes in cyclodeviation. By adjustment in the axis settings of the two Maddox rods they are made to appear parallel; thus the degree of cyclodeviation can be determined.
|
The Maddox rod test is particularly helpful in superior oblique palsy. Most commonly the paretic eye shows excyclotorsion on double Maddox rod testing, but if the patient fixates with the paretic eye, possibly the nonparetic eye will measure excyclotorsion.14 High amounts of excyclotorsion suggest bilateral superior oblique palsy. Although no absolute amount of excyclotorsion can be used to differentiate a unilateral from a bilateral superior oblique palsy, one study found a 90% probability of a superior oblique palsy being bilateral if the excyclotorsion measured in downgaze was greater than 20°.15 Mitchell and Parks16 suggested that 10° or more of excyclotorsion in the primary position was consistent with bilateral superior oblique palsy.
Red Filter.
While the patient fixates a small spot source of light, a red lens is placed before one of the eyes (Fig. 10). This test accomplishes the same thing as the Maddox rod in the horizontal and vertical deviations, but it is of no value in investigating cyclodeviations. It is less likely to disrupt fusion than the Maddox rod because only the color and the intensity of the images are made dissimilar whereas the contour of the images in the right and the left eye remains the same. The patient can fuse the white and the red light into a “pink” light. Prisms are used to eliminate the horizontal or vertical diplopia, yielding a direct measure of the deviation if the retinal correspondence is normal.
DISSIMILAR TARGET TESTS.
A number of different techniques for evaluating alignment are based on the presentation of different targets to the right and the left eye while the patient adjusts the projection device to superimpose the dissimilar images. If the retinal correspondence is normal, the point at which the images appear superimposed provides a direct reading of the patient's alignment. The two most widely used methods employing this principle are the Lancaster red-green projectors and the major amblyoscope.
Lancaster Red-Green Projectors.
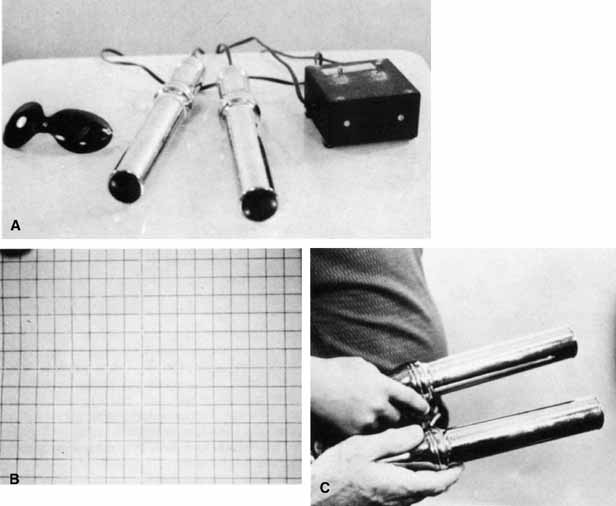
One projector shines a red target and the other a green target on a white screen marked with a grid calibrated in prism diopters; the screen is 1 meter from the patient. The targets, of similar contour and intensity, are viewed by the patient with red-green spectacles (red filter before one eye and green before the other). The patient adjusts the targets so they appear superimposed (Fig. 11), thus affording a direct reading of any deviation. Horizontal, vertical, and torsional deviations are well revealed because the targets are linear, 2 to 3 cm in length.17
Major Amblyoscope.
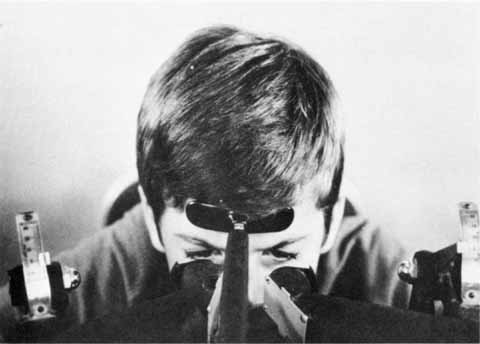
The patient views the dissimilar targets, which are simultaneously deposited in the housing of each tube, and adjusts them so that the images (e.g., bird and cage, car and garage, fish and bowl) are superimposed (Fig. 5, 6, and 7A). If the retinal correspondence is normal, the horizontal, vertical, and torsional deviations are read directly from the scales on the instrument that records the deflections of the tubes away from zero in these three planes. Furthermore, the illumination of the tubes can be alternately flashed on and off, allowing only one eye to view the target at a time. By observing the movement of the eyes as they fixate first one and then the other target, the examiner can adjust the tubes to eliminate all movement (Fig. 12). This, in effect, is an alternate cover test; however, instead of using prisms to measure the quantity of deviation, it is recorded by the scales on the instrument.
With the exception of testing methods using the major amblyoscope, primary position alignment may be investigated either while the head is erect or when it is tilted to either shoulder. The purpose of testing the alignment in the primary position with the head tilted is to study the effect of the utricular reflex in cyclovertical muscle deviations. The head is rotated about the coronal axis for 60° toward either shoulder, and the alignment is checked by cover tests, corneal reflex tests, dissimilar image tests, or the Lancaster red-green projectors.