WEAKENING OR STRENGTHENING HORIZONTAL RECTUS MUSCLES
Urist5,6 suggests weakening or strengthening the horizontal rectus muscles, claiming that the medial rectus muscles are most effective in midline downgaze because this is the usual position for convergence. He further claims that the lateral rectus muscles are most effective in midline upgaze because divergence is usually accomplished by looking upward from the downturned near-seeing position to see something at distance. By appropriately recessing or resecting these muscles to alter their power, not only is the horizontal measurement in the primary position improved, but also, theoretically, the A and V patterns are improved. For example, an ET-V pattern is improved with recessions of the medial rectus muscles, an ET-A pattern with resections of the lateral rectus muscles, an XT-V pattern with recession of the lateral rectus muscles, and an XT-A pattern with resections of the medial rectus muscles.
VERTICAL TRANSPOSITION OF HORIZONTAL RECTUS MUSCLES
Knapp23 conceived the idea of vertical transposition of the insertions of the horizontal rectus muscles, proved its effectiveness, and popularized its usefulness in treating A and V patterns. He reasoned that vertical transposition of the insertions of the horizontal rectus muscles alters their scleral attachment relative to the rotation center of the globe, thus increasing the arc of contact of the transpositioned muscle in one vertical gaze position and decreasing it in the opposite vertical gaze position. Because the pull power of the muscle is related to the stretch put on it by the arc of contact, the horizontal pull power is enhanced and diminished in opposite vertical gaze positions, as compared with the unoperated horizontal rectus muscle. Hence, the horizontal rectus muscles become more effective abductors or adductors in the vertical gaze position opposite the direction in which their insertions are moved. Stated differently, the transpositioned horizontal rectus muscles become less effective horizontal rotators in the same vertical gaze position as the direction in which they are moved. For example, the infraplaced medial rectus muscles are more effective adductors in upgaze than in downgaze, or the supraplaced lateral rectus muscles are less effective abductors in upgaze than in downgaze. Therefore, an ET-V pattern is improved with either recessions and infraplacement of the medial rectus muscles or recession-resection on one eye, which also infraplaces the medial rectus muscle and supraplaces the lateral rectus muscle.
The directions in which the horizontal rectus muscle are transpositioned for A or V patterns associated with horizontal tropia are summarized in Table 1. The consensus seems to be that the usual quantity of transposition is half the width of the tendon. Although some surgeons perform total-width transplants, they experience greater unpredictable results in horizontal alignment in the primary position. Half-width tendon transpositions yield 15Δ to 20Δ change in the A or V pattern between upgaze and downgaze. Full-width transpositions produce more improvement, but the unpredictability of the horizontal correction in the primary position plus frequent limitation of duction in the field of action of the transpositioned muscle limits the usefulness of this quantity of surgery. Sharma and colleagues24 concluded that a 5-mm shift was as effective as an 8-mm shift in monocular vertical displacement of horizontal rectus muscles in A and V patterns, even when mild or moderate cyclovertical muscle imbalance was present. However, in all cases with oblique muscle dysfunction, residual vertical incomitance was observed, and therefore, the authors recommended vertical shifting only when there was no associated cyclovertical muscle imbalance.
Table 1. Directions in Which the Horizontal Rectus Muscles
Are Transpositioned for Esotropic and Exotropic A and V Patterns
| Medial Rectus | Lateral Rectus | |
| ET-V |
↓
|
↑
|
| ET-A |
↑
|
↓
|
| XT-V |
↓
|
↑
|
| XT-A |
↑
|
↓
|
ET, esotropia: XT, exotropia.
Vertical transposition of the horizontal rectus muscles may be performed symmetrically and bilaterally, or surgery may be confined to one eye, with appropriate vertical displacement of the medial and lateral rectus muscles.1,25,26 The determination of the amount of horizontal surgery is the same whether or not monocular vertical displacement is performed,27 even though Knapp23 has suggested increasing the usual amount of horizontal surgery when vertically displacing the horizontal muscles. Postoperative torsional symptoms or significant torsional measurements have not been produced. Oblique muscle dysfunction associated with the A or V pattern is not changed by vertically offsetting the horizontal rectus muscles.
In a retrospective study of 67 patients, Scott and colleagues28 reported an initial correction of 96%, within ± 10Δ of pattern. The standard horizontal rectus muscle surgery combined with half-width tendon offsetting surgery of the horizontal rectus muscles was shown to be an effective operation for collapsing all subgroups of the A- and V-pattern strabismus with appropriate indications. With A and V patterns without significant oblique dysfunction requiring surgery, the authors advocated standard horizontal surgery with half-width tendon offsets in A and V patterns from 10Δ to 30Δ. If the pattern exceeded 30Δ, they recommended three-fourths to full-tendon–width offsets combined with the standard horizontal rectus muscle surgery. When oblique muscle dysfunction was present, they recommended appropriate oblique muscle strengthening or weakening procedures along with appropriate horizontal or vertical rectus muscle surgery.
WEAKENING OR STRENGTHENING VERTICAL RECTUS MUSCLES
Weakening or strengthening the vertical rectus muscles was tried for correcting A and V patterns but did not pass the test of time. The principle that precipitates this technique is the secondary adduction effect produced by the vertical rectus muscles in the primary position. The total adduction produced by these muscles theoretically increases as the inferior rectus muscles contract in downgaze and as the superior rectus muscles contract in upgaze.
Recession or resection of appropriate vertical rectus muscles29 reduces the A and V patterns. The changes produced are maximal in downgaze with surgery on the inferior rectus muscles and maximal in upgaze with surgery on the superior rectus muscles. The primary procedure recommended for the ET-V or A pattern is recession of the appropriate vertical rectus muscles: The inferior rectus muscles for the V pattern and the superior rectus muscles for the A pattern are recessed. If secondary improvement in the ET-V- or A-pattern measurements is desired, resections of the opposing unoperated vertical rectus muscles are performed. The XT-V or -A pattern requires resections of the appropriate vertical rectus muscles: resection of the superior rectus muscles for the V pattern and the inferior rectus muscles for the A pattern. Secondary improvement in the XT-V or -A pattern is obtained by recession of the opposing unoperated vertical rectus muscle (Table 2). Four-millimeter recessions and resections of the vertical rectus muscles are performed. The associated oblique muscle dysfunction is also improved by the surgery on the vertical rectus muscles. The horizontal deviation in the primary position remains unaltered by the surgery on the vertical rectus muscles; therefore, surgery is also required on the horizontal rectus muscles at this time.
Table 2. Primary and Secondary Surgery to Improve Esotropic
and Exotropic V or A Patterns
| Recession | Resection | |
| V | IROU | SROU* |
| ET | ||
| A | SROU | IROU* |
| V | IROU* | SROU |
| XT | ||
| A | SROU* | IROU |
*Secondary surgery.
IROU, inferior rectus muscle of both eyes; SROU, superior rectus muscle of both eyes.
Melek and colleagues30 described the influence of bilateral recession of the superior rectus muscles on A- and V-pattern strabismus. They concluded that this procedure tends to increase V patterns and reduce A patterns, and they stated that superior rectus recession may be synergistic with superior oblique tenotomy in collapsing an A pattern.
SLANTING MUSCLE INSERTIONS OF HORIZONTAL RECTUS MUSCLES
In 1971, Boyd and colleagues31 described a new technique of slanting the insertions of medial and lateral rectus muscles for recessions or resections in A and V patterns without overaction of vertically acting muscles. In V esotropia, the medial rectus muscles were recessed more inferiorly than superiorly, and in A esotropia, more superiorly than inferiorly. In V exotropia, the lateral rectus muscles were recessed more superiorly than inferiorly, and in A exotropia, more inferiorly than superiorly. The same technique was recommended for resections. The benefits included fewer induced torsional effects and less technical difficulty than with vertical transpositions. Except for papers by Biedner and Rothkoff32 and Ohba and Nakagawa,33 the literature remains sparse and this technique has not been generally accepted.
HORIZONTAL TRANSPOSITION OF VERTICAL RECTUS MUSCLES
Horizontal transposition of the vertical rectus muscles to correct the A and V patterns was first advocated by Miller.29 The adduction component of the vertical rectus muscles is enhanced or lessened, respectively, by transpositioning their insertions nasally or temporally, thus altering the effective moment of force of the contracting muscle relative to the rotation center of the globe. The change in horizontal alignment during downgaze is maximal with horizontal transposition of the inferior rectus muscles, and the upgaze is maximally affected with surgery on the superior rectus muscles. For example, to decrease excessive convergence in downgaze, as encountered in ET-V, the insertions of the inferior rectus muscles are transpositioned temporally. The directions for the horizontal transposition of the vertical rectus muscles to improve the A and V patterns are listed in Table 3. The usual quantity of horizontal transposition is half the width of the tendon; this does not interfere with the vertical duction of the operated vertical rectus muscle. The horizontal deviation in the primary position remains relatively unaltered by the horizontal transposition of the vertical rectus muscles; therefore, surgery on the horizontal muscles is also required and may be done at this time. Although transposition of the vertical rectus muscles received an adequate trial by many surgeons, its general abandonment as a method of treating A and V patterns resulted from its relative ineffectiveness.
Table 3. Directions for the Horizontal Transposition
of the Vertical Rectus Muscles to Improve A and V Patterns
| Nasally | Temporally | |
| SROU | XT-V | ET-A |
| IROU | XT-A | ET-V |
IROU, inferior rectus muscle of both eyes; SROU, superior rectus muscle of both eyes; XT, exotropia; ET, esotropia.
WEAKENING OR STRENGTHENING OBLIQUE MUSCLES
Weakening or strengthening oblique muscles is used by most surgeons to improve the A and V patterns. The rationale for this surgery stems from the secondary abducting action of these muscles; this action is classically considered to be present minimally in the primary position for both inferior and superior oblique muscles. The inferior oblique muscles become stronger abductors in upgaze than in downgaze, and the superior oblique muscles become stronger abductors in downgaze than in upgaze. Consequently, the V pattern is improved either by weakening the inferior oblique muscles or by strengthening the superior oblique tendons; the opposite is done for the A pattern (Table 4). Because weakening procedures on the oblique muscles consistently improve the A and V patterns, they have great popularity. However, the weakening procedures are indicated only for overacting oblique muscles; this overacting may be lacking in A and V patterns. Weakening normal oblique muscles produces an underaction easily detectable in version testing; this is obviously an undesirable result.
Table 4. Weakening and Strengthening Procedures on Oblique
Muscles to Improve A and V Patterns
| Weakening | Strengthening | |
| V | IOOU | SOOU |
| A | SOOU | IOOU |
IOOU, inferior oblique muscle of both eyes; SOOU, superior oblique muscle of both eyes.
Strengthening procedures on the oblique muscles are less dependable than weakening procedures and, consequently, are rarely performed. Resecting and advancing the insertions of the inferior oblique muscles nets little improvement in the A pattern and insignificant reduction in the preoperative overacting superior oblique muscles. Tucking the superior oblique tendons temporal to the superior rectus muscles causes reduction in the preoperative overelevation of the eyes (resulting from overacting inferior oblique muscles), but this procedure often causes a postoperative vertical deviation and an obvious incyclodeviation in the primary position that was nonexistent preoperatively. Although the V pattern is improved by strengthening the superior oblique tendons, the same result can be achieved by weakening the inferior oblique muscles, with less hazard to the patient. Therefore, bilateral weakening procedures on the inferior oblique muscles are more popular than bilateral strengthening procedures on the superior oblique tendons.
Weakening the inferior oblique muscles corrects 15Δ to 25Δ of the V pattern between primary position and upgaze, depending on the severity of the overaction of the muscles. The surgery does not alter the lower component of the V pattern between primary position and downgaze. Also, the horizontal alignment of the eyes in the primary position remains relatively unchanged,34,35 which is contradictory to the earlier principle that weakening the secondary abductors produces a relative convergence of 5Δ to 10Δ. Bilateral recession of overacting inferior oblique muscles is associated with a favorable prognosis, eliminating the overactions and not producing a cyclovertical imbalance in the primary position.36 Almeida and Alvares37 recommended split lengthening of the inferior oblique muscles in unilateral or bilateral surgery for V pattern as a method to avoid torsional deviation, which the authors felt could occur with recession. However, because of the possibility of excessive bleeding from the muscle splitting, the need for generous intraoperative cautery, the complexity of split lengthening of the inferior oblique, and the possibility of postoperative scarring, the less-complicated inferior oblique recession or other weakening procedures are the treatments of choice.
Graded anterior transposition of overactive inferior oblique muscles has been shown by Guemes and Wright38 to be effective in normalizing versions and in correcting vertical deviations in the primary position. The inferior oblique is reattached to the sclera at various points along the temporal border of the inferior rectus muscle, with increased anteriorization with increased degrees of inferior oblique overaction. When this technique was applied to V-pattern strabismus, Monteiro de Carvalho and colleagues39 reported a success rate of 75% in 53 cases, with a residual V pattern of 8Δ or less. Polati and Gomi40 reported a 77.3% reduction in V pattern to less than 10Δ in 44 procedures.
Weakening the superior oblique muscle is accomplished by tenotomy along the nasal border of the superior rectus muscle. By simple transection of the tendon, leaving it attached to the surrounding intermuscular septum, 25Δ to 45Δ of the A pattern is eliminated. Contrary to prior observations and opinions, sectioning the tendons of both eyes without opening Tenon's capsule farther than 10 mm from the limbus does not significantly alter the primary position horizontal alignment. Formerly it was observed that bilateral tenotomy, using the technique in which Tenon's capsule was extensively opened 20 mm or more posterior to the limbus, converged the primary position horizontal alignment 15Δ to 20Δ and left the top of the A (upgaze) unchanged.41–43 Now, with the more modern tenotomy technique, the change in horizontal alignment is symmetrical in upgaze and downgaze, without significant esoshift in primary position, as shown in independent studies by Parks,44 Pollard,45 Fierson and co-workers,46 Diamond and Parks,47 and Prieto-Diaz.48
This procedure should not be used unless the A pattern is at least 25Δ and is associated with overacting superior oblique muscles, and the patient is either a monofixator or has anomalous retinal correspondence binocular vision or no binocular vision. The surgeon should avoid performing tenotomy of the superior oblique muscles if the patient is capable of bifixation (central fusion with excellent stereoacuity). A patient who has an A pattern and overacting superior obliques and who bifixates when the eyes are straight usually has intermittent exotropia. A patient who bifixates will be much more annoyed about a persistent primary incyclodiplopia caused by the resultant excyclodeviation following bilateral superior oblique tenotomy than will either a monofixating patient or a patient with anomalous retinal correspondence. Patients without binocular vision will have no postoperative diplopia. A bifixating patient with postoperative excyclodeviation and torsional diplopia tends to depress the chin and keep the eyes in upgaze, thus diminishing the deviation and compensating for the diplopia. Also, with the best surgical technique, it is not unusual to obtain a greater weakening effect on one tenotomized superior oblique muscle than on the other, thus causing a vertical deviation in the primary position and the typical cardinal field findings and Bielschowsky's head tilt findings in a unilateral superior oblique palsy. The ensuing torticollis adopted by the patient corrects the primary position postoperative cyclovertical deviation. This outcome is only likely to occur in a bifixating patient, who happens to be almost invariably a patient with intermittent XT.
Although one of the authors of this chapter (MMP) has for 40 years cautioned against performing bilateral superior oblique muscle tenotomies in patients with intermittent XT, this advice has usually gone unheeded. A convincing case report by Rubin and colleagues49 documents postoperative torsional diplopia in the primary position that could be eliminated by maintaining chin depression, following tenectomy of the superior oblique muscles by one of the authors in a bifixating patient with intermittent XT. The patient was operated by MMP, who found the 6-mm tenectomized tendons had rejoined with scar tissue between the proximal and distal ends. A Harada-Ito procedure eliminated the excyclodeviation, chin depression, and torsional diplopia. Although the surgically induced symptoms were finally corrected by repeat surgery, the better course would have been to avoid bilateral superior oblique muscle surgery for A pattern in a patient who has bifixation postoperative potential.
Of the six surgical methods described to treat the A and V patterns, only two receive widespread acceptance: vertical transposition of the insertions of the horizontal rectus muscles and weakening of the oblique muscles. Some consideration is given to the realization that recessions of the medial rectus muscles slightly improve the V pattern and aggravate the A pattern.
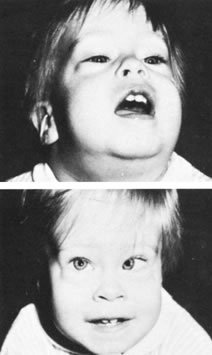
In patients with ET-A, the chin is often elevated, maintaining the eyes in downgaze (Fig. 1). Purposely avoiding recessions of the medial rectus muscles and performing resections and infraplacement of the lateral rectus muscles failed in correcting both the ET and the A patterns. Recession of the medial rectus muscles, despite aggravating the A pattern, is necessary to improve the ET, and simultaneous supraplacement of the insertions prevents aggravation of the A pattern. This procedure has become the standard surgical approach for patients with ET-A of slight to moderate degree; it corrects approximately 15Δ of A pattern. Large A patterns associated with ET are rare, and they are usually associated with underaction of the inferior oblique muscles and overaction of the superior oblique muscles. Tenotomy of the superior oblique tendons overcomes approximately 40Δ of A pattern, without altering the primary position horizontal deviations.
|
|
Knapp18 has reported advancement and resection of the inferior oblique muscles with satisfactory results in three cases, although there was marked reaction to the surgery. In more exaggerated cases of ET-A, Goldstein50 reported bilateral inferior oblique advancement as an effective alternative procedure for management.
In patients with ET-V, the chin is often depressed, maintaining the eyes in upgaze (Fig. 2). Simply recessing the medial rectus muscles corrects approximately 10Δ of V pattern. Also, infraplacement of the insertions of the medial rectus corrects an additional 15Δ of V pattern. Recession of associated overacting inferior oblique muscles corrects another 15Δ of V pattern between the primary position and upgaze. Therefore, presuming the ET-V has associated overacting inferior oblique muscles, recessions and infraplacements of the medial rectus muscles combined with recessions of the inferior oblique muscles correct up to 45Δ of V pattern.
|
|
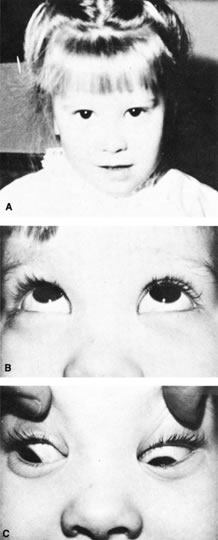
Patients with XT-A frequently have depressed chin compensatory head posture, and they keep the eyes elevated in fusing (Fig. 3). They can receive 15Δ to 20Δ of A-pattern correction with recessions of the lateral rectus muscles and infraplacement of their insertions. However, if greater A-pattern correction is required and overaction of the superior oblique muscles is apparent, the surgeon may wish to tenotomize the tendons of these muscles. Because tenotomy of the superior oblique tendons corrects 40Δ of A pattern without affecting primary position deviation, the quantity of exosurgery need not be adjusted if the lateral rectus muscles and superior oblique tendons are operated on simultaneously. Furthermore, combining infraplacement of the lateral rectus muscles with tenotomy of the superior oblique tendons would require that the patient have 60Δ of A pattern preoperatively, which is rather unusual. Therefore, the usual treatment of patients with XT-A is simply infraplacement of the recessed insertions of the lateral rectus muscles if the A pattern is less than 40Δ or tenotomizing the superior oblique tendons if the A pattern is 40Δ to 55Δ and if the superior oblique muscles are overacting.
|
|
Surgeons should experience some uneasiness about tenotomizing the superior oblique tendons in a patient with intermittent XT for fear that the surgery will produce a postoperative imbalance in the primary position of the cyclovertical muscles with cyclovertical diplopia that is compensated for by tilting the head. Surgeons may prefer to disregard the large A pattern and the overacting superior oblique muscles in intermittent XT, merely correct the primary position exoangle with combined recessions and infraplacements of the lateral rectus muscles, and accept whatever residual A pattern persists. If secondary surgery is required to correct the exoangle and if 15Δ or more of the A pattern remains, the medial rectus muscles are resected and their insertions are supraplaced at this time. Tenotomy of the superior oblique tendons in patients with constant XT without binocular vision potential, having 40Δ or more of A pattern, and with overacting superior oblique muscles carries only minimal risk of postoperative torticollis.
Patients with XT-V frequently have chin elevation to permit fusion with downturned eyes (Fig. 4). Surgery for XT-V correction is managed differently, depending on the presence or absence of associated overacting inferior oblique muscles and the quantity of the V pattern. If present, the associated overacting inferior oblique muscles are always recessed simultaneously with the lateral rectus muscles. This eliminates 15Δ to 25Δ of V pattern according to the severity of the overactions of the inferior oblique muscles, but the correction is only between primary position and upgaze. The inferior oblique muscles are never weakened if they are not overacting. Combining supraplacement with recessions of the lateral rectus muscles corrects 15Δ to 20Δ of V pattern. If it is necessary to correct more of the V pattern, the insertions of the medial rectus muscles can be infraplaced to provide an additional 15Δ to 20Δ of correction.
|
|
A and V patterns also occur in the absence of a horizontal deviation in primary position, causing a tropia in upgaze or downgaze. Oblique muscle overactions are usually associated with these types of A and V patterns. Overacting inferior oblique muscles are recessed in these patients, and the upper half of the V pattern is improved. However, tenotomies of superior oblique tendons in patients with overacting superior oblique muscles are associated with the high risk previously alluded to regarding the imbalance in the primary position of the cyclovertical muscles that causes torticollis postoperatively. The insertions of the horizontal rectus muscles may be vertically displaced without simultaneous recession or resection in order to improve the A or V pattern in these patients. Also, within this group of patients, one occasionally encounters a V-pattern accommodative patient who has ET and whose eyes are straight with plus spectacles at distance but who has ET at near as a result of a high accommodative convergence to accommodation (AC : A) ratio. Placing +2.50 lenses in a trial frame controls the near ET, but the near ET persists with bifocals because the patient must depress his or her eyes to use them. The V pattern causes the ET in downgaze, although the lower segment of the bifocal disengages the accommodation. In such a patient, the combination of the high AC : A ratio and the V pattern makes bifocals useless. Either a miotic must be used instead of the bifocals or the medial rectus muscles must be infraplaced to help this patient. The opposite of this disorder is the A pattern occurring in downgaze with straight eyes at distance and near. Symptoms are caused by the exophoria that occurs when the eyes depress to do near work. These symptoms are relieved only by holding the near work up to eye level or by flexing the chin on the chest while doing the near work. The condition in such patients is improved by supraplacement of the insertions of the medial rectus muscles without a combined recession or resection.
V-PATTERN STRABISMUS WITH CRANIOFACIAL DYSOSTOSIS
In cranial dysostosis, V-pattern strabismus with severe oblique muscle dysfunction is the most commonly seen motility problem51 and is complex and difficult to cure with surgery. Myectomy of the inferior oblique muscle or denervation/extirpation of the inferior oblique produced modest benefits, without any patient achieving normalization of ocular motility. Medial rectus infraplacement and inferior oblique anterior transposition did not produce beneficial effects. In many of the affected patients, agenesis of the superior oblique tendon may be causally related.51