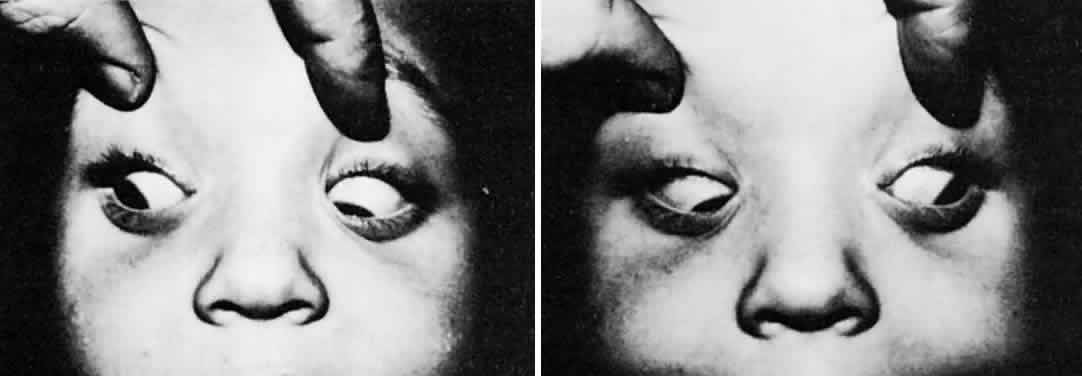
The primary and secondary overactions of the inferior oblique muscles have different clinical presentations. Although the patient with primary overaction of the inferior oblique muscle presents with an overelevated adducted eye, there is little vertical deviation in the primary position (Fig. 1). The vertical deviation appears to be the only manifestation of the overacting muscle. An overacting cyclodeviation element is not clinically apparent. It probably would be more accurate to refer to primary overaction of the inferior oblique muscle as overelevation of the adducted eye.
|
In contrast, the overacting inferior oblique muscle secondary to a palsy of the superior rectus muscle in the opposite eye or of the superior oblique muscle in the same eye is associated with a significant vertical deviation in the primary position plus a manifest excyclodeviation. Although the cyclodeviation is present in the primary position, it is maximal in abduction.
Cyclodeviation may be measured subjectively by the double Maddox Rod test, Lancaster red-green test, haploscopic methods, and the Maddox Wing test. Anatomic measurements include indirect ophthalmoscopy, fundus photography, and blind-spot mapping.1
The vertical deviation in the primary position in secondary overaction of the inferior oblique muscle usually ranges between 10Δ and 25Δ and the excyclodeviation from 5° to 10°. Consequently, the patient with secondary overaction of the inferior oblique muscle has sufficient imbalance in both cyclodeviation and vertical elements with the contralateral superior rectus muscle or the ipsilateral superior oblique muscle to produce a positive Bielschowsky head tilt test.2 In contrast, the isolated vertical element involvement in primary overaction of the inferior oblique muscle is associated with a vertical deviation in the primary position of between 0Δ and 5Δ and zero excyclodeviation. Furthermore, on tilting the head toward the right or the left shoulder, neither the vertical alignment changes nor an excyclodeviation is produced.
Histopathologic study of overactive inferior oblique muscles obtained at surgery did not demonstrate any abnormality on conventional hematoxylin-eosin staining.3 Histochemical and electron microscopic studies, however, revealed remarkable changes in the muscle fibers of the overactive inferior oblique muscle, demonstrating central cores, 100 μm to 150 μm long, in the orbital side of the muscle containing small-diameter muscle fibers that were highly positive in succinic dehydrogenase and lactic dehydrogenase activity. Aggregates of packed mitochondria were the constituents of these cores on electron microscopy, suggesting myopathic alteration of the inferior oblique muscles. Meyer and coworkers4 reported similar findings, with huge accumulations of mitochondria and muscle vacuolization related to the enlargement of the tubules of sarcoplasmic reticulum. These mitochondrial aggregates and vacuoles occupied more inferior oblique muscle surface in the primary overactive rather than secondary overactive inferior oblique muscles.
In an electron microscopic study5 of overacting inferior oblique muscles—both primary and secondary—the most striking abnormalities were aggregations of mitochondria and degenerating mitochondrial profiles and increased vacuolization in primary and secondary overacting muscles. The muscle fibers were in different stages of atrophy, and hypertrophy and regeneration of muscle fibers were visible, suggesting that primary overacting inferior oblique muscles may be secondary to paresis of the superior oblique muscle.
PRIMARY OVERACTION
Primary overaction of the inferior oblique muscle apparently is not congenital. Rarely can the onset of this condition be recorded before 1 year of age. More commonly, onset is after 1 year of age; this condition may appear at any time during the first several years, most frequently between 2 and 4 years of age.
Primary overaction of the inferior oblique muscle may be an isolated motility disorder or it may occur in conjunction with a horizontal deviation of the eyes. It seems to occur with equal frequency in patients with esotropia and in patients with exotropia. It appears with equal frequency in patients with congenital esotropia and in those with acquired esotropia. Furthermore, intermittency of the horizontal deviation does not seem to influence the frequency of this disorder. It occurs with about equal frequency in patients with intermittent exotropia and in those with constant exotropia.
Wilson and Parks6 performed a statistical analysis of the onset and natural history of primary inferior oblique overaction in 456 strabismus patients. With 5 or more years of follow-up, 72% of patients with congenital esotropia, 34% of patients with accommodative esotropia, and 32% of patients with intermittent exotropia developed inferior oblique overaction at an average age of 3, 6, and 5.2 years, respectively. There was a positive correlation to the number of horizontal surgeries in congenital esotropia but not in the other groups. The incidence of overactive inferior oblique muscles was not related to the age at onset of strabismus, time from onset of strabismus to surgery, age at first surgery, or decompensation of ocular alignment.
Primary overaction of the inferior oblique muscle may have its onset equally in the two eyes or it may occur only in one eye. After developing in one eye, it may gradually develop in the opposite eye. The dissimilarity in the degree of the overaction of the inferior oblique muscles may be temporary; with time, the degrees of overaction in the two muscles may gradually become equal. Unilateral overaction of the inferior oblique muscle occurs with sufficient frequency that the clinician is unable to make the statement that if one inferior oblique muscle overacts, eventually both will overact. In patients with unilateral overactive inferior oblique muscles, Raab and Costenbader7 found that the normal second inferior oblique muscle developed significant overaction in about a third of cases after unilateral inferior oblique weakening. In the presence of even the slightest overaction in the nonoperated inferior oblique, unilateral weakening of the overactive inferior oblique was followed in two thirds of cases by worsening of the nonoperated inferior oblique by 2 to 6 months postoperatively. Overaction of the second inferior oblique usually begins within 2 to 6 months of the onset of overaction of the first inferior oblique muscle, whether or not inferior oblique weakening surgery was performed on the eye with the more prominent overactive inferior oblique.
Primary overactions of the inferior oblique muscles that are unassociated with any horizontal deviation of the eyes do not disturb the single binocular vision in the primary position. Depending on the degree of overaction, there is a measurable midline zone of varying size within which the eyes may make horizontal excursions and not disturb the binocular vision. The maximal horizontal excursion that is possible before the gradually increasing vertical phoria transforms to vertical tropia is recorded as the fusion breakpoint, however. At this point, diplopia is encountered. The patient usually responds by subconsciously limiting the horizontal movement of the eyes to the extent that diplopia is avoided. Consequently, on viewing sideways, the patient is more apt to turn the head toward the position desired for seeing than to turn the eyes, except when startled by a visual or auditory stimulus located off to the side beyond the diplopic threshold.
Primary overactions of the inferior oblique muscles associated with a horizontal deviation are one of the mysteries of motility. It is often stated that the longer the duration of the horizontal deviation the greater the tendency for oblique muscle dysfunction. The congenitally esotropic infant, however, who at a young age had excellent surgical correction of the horizontal deviation has the same chance of developing overaction of the inferior oblique muscles some years after the surgery as the congenitally esotropic patient who receives no surgery to correct the horizontal deviation until adulthood. Early corrective surgery for congenital esotropia does not diminish the chance that the congenital esotrope will develop overacting inferior oblique muscles. According to the one study,8 about 65% of congenitally esotropic patients are destined to develop overacting inferior oblique muscles. Hiles and coworkers9 reported a 78% incidence of inferior oblique overaction in one or both inferior oblique muscles during their study of 54 patients with congenital esotropia. Similarly, elimination of intermittent exotropia at a young age does not preclude future development of primary overacting inferior oblique muscles. Correction of the accommodative esotropia soon after onset with spectacles does not lessen the chance for later development of primary overacting inferior oblique muscles. Therefore, one should question the statement that the longer the duration of the horizontal deviation, the greater the chance of oblique muscle dysfunction.
Weakley and coworkers10 studied 368 patients with infantile esotropia, acquired accommodative or partially accommodative esotropia, or acquired nonaccommodative esotropia. Of the 126 patients (34%) with amblyopia, 93 patients (74%) had symmetric inferior oblique overaction; however, 31 patients (25%) had more inferior oblique overaction in the eye with the amblyopia. The authors stress that asymmetric inferior oblique overaction in esotropia correlates highly with amblyopia in the eye with greater inferior oblique overaction, regardless of the subtype or duration of the esotropia or the angle of deviation.
Eustis and Nussdorf11 photographed the posterior pole at the time of surgery in 27 eyes of 14 patients with infantile esoptropia. A masked observer graded each photograph for the presence or absence of fundus torsion. Of the 27 eyes, 15 developed inferior oblique overaction and 6 of the 15 demonstrated fundus excyclotorsion before the inferior oblique overaction was clinically recognized. Therefore, the presence of fundus torsion with infantile esotropia may serve as a marker or predictor of subsequent overt inferior oblique overaction.
Primary overaction of the inferior oblique muscles is frequently associated with a V pattern. In patients with congenital esotropia, the overacting inferior oblique muscles are usually associated with dissociated vertical deviation or hypertropia. In some patients, the differentiation between overaction of the inferior oblique muscles and dissociated vertical deviation is difficult. When the eyes are horizontally deviated to the extent that the visual axis of the adducted eye is interrupted by the nose, the eye deviates upward. This can simulate overaction of the inferior oblique muscle to the extent that in some patients it is impossible to make the differentiation.
The treatment of an overacting inferior oblique muscle is to weaken it surgically. Primary overaction of the inferior oblique muscle is not associated with an excyclodeviation, and weakening this primarily overacting muscle does not produce an incyclodeviation. Likewise, primary overaction of the inferior oblique muscle does not produce a significant vertical deviation in the primary position, and surgically weakening this primarily overacting muscle does not produce a vertical deviation in the primary position. Furthermore, unilateral primary overaction of the inferior oblique muscle is not associated with a positive Bielschowsky head tilt test, and this muscle does not produce a positive Bielschowsky head tilt test after the weakening procedure. In all of these respects, the primarily overacting inferior oblique muscle differs from the secondarily overacting inferior oblique muscle. The V pattern that may be associated with overacting inferior oblique muscles is improved by weakening these muscles, particularly between primary position and upgaze.
The inferior oblique muscles have a supposedly secondary abduction action when they contract to move the eyes from the primary position. For many years, allowances were made for a change in the horizontal alignment when the inferior oblique muscles were weakened. The exodeviation was claimed to be improved by 5Δ to 10Δ, and the esodeviation was worsened by 5Δ to 10Δ in patients in whom the primary overacting inferior oblique muscles were weakened. Stager and Parks12 have proved this claim to be erroneous. In effect, there is no significant change in the horizontal alignment of the eyes produced in the primary position by weakening procedures on primary overacting inferior oblique muscles.
In a prospective study, Parks13 investigated the various weakening procedures of the inferior oblique muscles and concluded that the recession procedure was the superior method. As early as 1947, Fink14 advocated surgery at the origin rather than the insertion of the inferior oblique muscle because of the ease of the approach and the nature of the anatomy and because the degree of effect was more readily controlled when approached at the inferior oblique insertion. The poorest method of inferior oblique weakening is a myectomy between the origin and the nasal border of the inferior oblique muscle. This technique is inadequate because of the significant recurrence of the overacting inferior oblique muscle, which required secondary surgery in 32% of the patients. Three types of surgical weakening procedures were performed on the insertional portion of the inferior oblique muscle temporal to the inferior rectus muscle: (1) recession; (2) disinsertion, allowing the muscle to seek its own insertional site; and (3) myectomy between the temporal border of the inferior rectus and the muscle insertion. Disinsertion has been advocated as an effective, reliable, safe, and fast procedure.15,16 Parks,13 however, found that a tendency for recurrence of the overaction of the surgically weakened insertion end of the inferior oblique muscle was greatest with disinsertion, whereas the result of myectomy was between those produced by disinsertion and recession. Repeat surgery disclosed that the disinserted or myectomized muscle had reattached to the original insertion site in most patients.
Internal ophthalmoplegia of months to years in duration after inferior oblique myectomy has been reported.17,18 Careful surgical dissection has revealed that the easiest way to locate the ciliary ganglion is to first locate the nerve to the inferior oblique muscle that runs parallel and close to the lateral border of the inferior rectus muscle and to follow it backward to the motor root of the ciliary ganglion.19 Internal ophthalmoplegia should also be a rare occurrence with recession or denervation and extirpation of the inferior oblique, although this complication has yet to be reported in the literature.
The worst complication occurring in patients whose overacting inferior oblique muscles are weakened is the adhesive syndrome.13 This syndrome is manifest by gradual development of hypotropia in the primary position in a patient without vertical deviation before surgery on the inferior oblique muscle.
The hypotropia gradually increases over a period of several months to several years and produces as much as 35Δ of vertical deviation. Furthermore, the patient is unable to elevate the hypotropic eye, and the traction test is positive for resistance to elevation of this eye. On surgical exploration of the hypotropic eye, the inferior oblique is not found to be the cause. Instead, it is Tenon's capsule in the inferior temporal region, which is thickened by fibrofatty proliferation and scarring to the sclera. This fibrofatty tissue extends to the temporal side of the capsule of the inferior rectus muscle and is attached firmly to the muscle near its insertion. Presumably, cicatrization of the fibrofatty tissue, extending between the tissue of the inferior temporal fornix and the insertional temporal end of the inferior rectus muscle, gradually drags the involved eye farther and farther downward, causing the increasing hypotropia and diminishing active and passive elevation that are particularly obvious in abduction.
Surgical improvement of the adhesive syndrome is difficult; this disorder invariably requires secondary surgery on vertical rectus muscles after the liberation of the involved inferior rectus from scarred Tenon's tissue and surrounding attachment of this muscle to the sclera. The adhesive syndrome is not related to a particular surgical procedure, as was originally thought when the adhesive syndrome resulting from inferior oblique surgery was described.13 Parks encountered it in 13% of the insertional myectomies, 2% of the disinsertions, and none of the recessions or myectomies between the origin of the muscle and the inferior rectus. But additional information revealed the true cause to be a violation of Tenon's capsule during the dissection of the muscle along its posterolateral border. A tear in Tenon's capsule results in scarring of the septae within the extraconal fat pad to the sclera and muscle capsules in the inferotemporal sub-Tenon's space.20
The surgeon performing the weakening procedure should possess adequate skill and knowledge of technique and anatomy to make certain that the entire muscle is dissected and that Tenon's capsule, containing the intramuscular fat pad, is not opened. Adequate view of the entire insertion can be easily achieved with a sustained adducted and elevated positioning of the eye; this is easily accomplished with a 4-0 silk-stay suture under the lateral rectus muscle attached to the drapes with hemostats. Exposure with a Desmarres or a Conway lid retractor over the insertional site of the inferior oblique is possible through an incision in the inferior temporal fornix; this allows the surgeon to lift the inferior oblique muscle out of its bed near its insertion by direct visualization rather than blindly sweeping a muscle hook under Tenon's capsule. The blind sweeping procedure has resulted in inadvertent myotomy and myectomy of both the lateral rectus and the inferior rectus muscles. Therefore, elevation of the inferior oblique muscle under direct vision, observation of the total insertion of the muscle, and weakening of the muscle produce significant improvement and do not harm the patient's eye alignment in the primary position.
A 10-mm recession of the inferior oblique muscles may produce an overcorrection in slightly overacting inferior oblique muscles. Therefore, slight overaction of the inferior oblique muscles requires relatively fewer millimeters of recession—that is, about 6 mm. Occasionally, primary overaction of the inferior oblique muscles recurs, even after 10 mm of recession. In this case, a further recession procedure is usually not helpful; myectomy of the inferior oblique muscle between the origin and the nasal border of the inferior rectus muscle also does not alter the trend of the recurrence of the overaction. Gonzalez21 reported initial success in reducing overaction of the inferior oblique muscle by denervation. Subsequent studies,22,23 however, revealed reinnervation of the nerve to the inferior oblique, often with a greater vertical deviation than that present before the initial surgery. Further surgery, including denervation and myectomy, was required to effect a cure of the overaction. The only procedure that eliminates return of the overaction in this type of patient is denervation and partial extirpation of the inferior oblique muscle,24,25 which has not produced any vertical deviation in the primary position. Even more surprising is that the operated eye still elevates in adduction. Also, incyclodeviation does not remain more than a few weeks in the operated eye.
If the patient has unilateral primary overaction of the inferior oblique muscle, only this muscle is recessed. If the patient has asymmetric overaction of the inferior oblique muscles, then asymmetric surgery is performed. Overactions may be graded as slight (1+ ), moderate (2+ ), marked (3+ ), and severe (4+ ). The overactive inferior oblique is recessed 6 mm for slight overaction, 10 mm for moderate overaction, and 14 mm for marked overaction. A denervation and extirpation procedure is recommended for severe overaction.24,25 An inferior oblique muscle that is not overacting preoperatively is never recessed. The principle that the surgeon should always weaken both inferior oblique muscles because eventually the unaffected muscle will overact should be questioned. Undoubtedly a large percentage of patients having a unilateral overacting inferior oblique muscle that requires surgery will demonstrate overaction in the opposite inferior oblique muscle soon after surgery on the first eye. If the anticipated overaction of the normal inferior oblique muscle does not occur after surgery on this normal muscle, however, a significant underaction of this inferior oblique muscle may be evident after surgery.17 Furthermore, bilateral weakening procedures on only a unilateral overacting inferior oblique muscle produce a vertical deviation in the primary position unless a change occurs soon after surgery that is equivalent to the development of an overaction in the muscle that was normal before surgery. Not all normal inferior oblique muscles undergo this change, however, and in those that do not, the induced vertical deviation persists in the primary position.
Apt and Call26 enhanced the weakening effect of the recessed inferior oblique when they “bunched up” the posterior border of the recessed inferior oblique muscle toward the anterior border, using only one scleral suture for reattachment rather than reattaching the inferior oblique to the muscle at its full width to the sclera. A modification of the standard recession procedure is recommended by Scott27 and by Elliott and Nankin,28 with anterior transposition of inferior oblique after the usual disinsertion from the globe as in the normal recession procedure. Success has been reported with persistent inferior oblique muscle overaction after recession surgery and with marked inferior oblique muscle overaction as the initial surgical procedure.
Weakening procedures on the inferior oblique muscles are combined with surgery on the horizontal muscles when the misalignment is a combination of horizontal tropia and overaction of the inferior oblique muscles. There is no reason to perform separate procedures for the two different conditions.
The rare presentation of A-pattern esotropia with paradoxic overaction of the inferior oblique muscles is described by von Noorden and Olsen,29 Rosenberg and colleagues30 and by Khawam and Traboulsi.31 Treatment consists of inferior oblique weakening and medial rectus recession with supraplacement.
SECONDARY OVERACTION
Secondary overacting inferior oblique muscles are the result of secondary changes—that is, hypertrophy or contracture. Hypertrophy occurs in the inferior oblique muscle when its yoke (contralateral superior rectus muscle) is palsied and the palsied eye is preferred for fixation. For example, in the patient with palsy of the right superior rectus muscle and a dominant right eye, the left inferior oblique muscle receives excessive innervation. The chronic hypertonus caused by excessive innervation produces hypertrophy of this muscle.
Contracture results in the inferior oblique muscle when it is the direct antagonist of the paretic ipsilateral superior oblique muscle and the uninvolved eye is preferred for fixation. For example, in the patient with palsy of the left superior oblique muscle and a dominant right eye, the tone of the left inferior oblique muscle in the primary position is not offset by the weak antagonistic tone of the left superior oblique muscle. Consequently, the globe persistently remains elevated and the left inferior oblique muscle is persistently more contracted than the left superior oblique muscle; this causes the left inferior oblique muscle to become shortened.
Regardless of whether there is hypertrophy or contracture of the secondary overacting inferior oblique muscle, a significant vertical deviation develops in the primary position that increases in the field of vertical action of the inferior oblique muscle. There is also an excyclodeviation in the primary position. A V pattern is usually associated with the secondary overacting inferior oblique muscle.
The secondary overacting inferior oblique muscle requires time to develop after the onset of the palsied superior rectus muscle or the superior oblique muscle. Usually, the time required to produce this change exceeds 6 months, although there are exceptions; some patients show the earliest signs of hypertrophy or contracture of the inferior oblique muscle within several weeks after the onset of the palsy.
The treatment of secondary overaction of the inferior oblique muscle is to weaken it, and the ideal procedure is recession. This should be performed before tucking the palsied superior oblique tendon or resecting the palsied superior rectus muscle. Also, recession of the hypertrophied or contracted inferior oblique muscle should be performed before weakening the yoke muscle.
After superior oblique palsy with inferior oblique muscle overaction, anterior transposition of the inferior oblique muscle has been attempted to weaken the inferior oblique overaction.32 The inferior oblique was converted from an elevator to a depressor, however, and primary position hypotropia resulted, with diplopia and limitation of upgaze. Subsequent retrodisplacement of the inferior oblique muscle was required to eliminate the diplopia. It was thought that this procedure may be beneficial in the treatment of dissociated vertical deviations in association with overaction of the inferior oblique.
Stager and associates33 describe clinical, radiologic, and histologic evidence that the neurovascular bundle supplying the inferior oblique muscle serves as the functional origin of the inferior oblique after anterior transposition of the insertion and con erts the distal portion of the inferior oblique muscle from an elevator to a depressor. Stager and Weakley34 describe a new surgical approach for management of recurrent inferior oblique overaction after the anterior transposition procedure. A myectomy of about 1 cm or more of a portion of the inferior oblique, nasal to the inferior rectus, is performed, using a temporal incision and approach. This preserves the distal inferior oblique fibers attached to the neurovascular bundle, which provide the depressor function of the inferior oblique in its anterior transposed position.
Burke and coworkers35 also found anterior transposition of the inferior oblique to be an effective treatment for dissociated vertical deviation with inferior oblique overaction, but long-term results may be less stable if the preoperative dissociated vertical deviation is in excess of 15 prism diopters. Milot and colleagues36 confirm the effectiveness of the anterior transposition of overactive inferior oblique muscles with coexisting dissociated vertical deviation in a series of 27 procedures.
Ziffer and associates37 suggest that the anterior transposition converts the inferior oblique muscle from an elevator to a depressor on attempted elevation. Because of its powerful weakening ability, the anterior transposition should be reserved for patients with moderate to severe inferior oblique muscle overaction and should be performed on both eyes to avoid postoperative hypotropia in upgaze. Gonzalez and Cinciripini38 propose the anterior transposition procedure for treatment of unilateral superior oblique palsy. None of their three patients developed primary position hypotropia but all demonstrated some elevation deficiency, with elevation of the lower lid in upgaze.
In a series of 21 patients receiving an anterior transposition of the inferior oblique with overaction of the inferior oblique and dissociated vertical deviation, Seawright and Gole39 reduced the preoperative incidence of inferior oblique overaction from 84% to 16% postoperatively. Inferior oblique overaction was absent in 43% and improved in 86% of eyes. At the latest postoperative visit, 57% did not demonstrate any evidence of dissociated vertical deviation and 68% of eyes had no or improved dissociated vertical deviation. There was no evidence of primary position hypotropia in any patient who had unilateral anterior transposition, and there was no evidence of inferior oblique underaction. Three patients required repeat inferior oblique surgery.