1. Fresnel, cited by Miller OE, McLeod JH, Sherwood WT: Thin sheet plastic
Fresnel lenses of high aperture. J OptSocAm 41:807, 1951 2. Woodward F: Unlikely looking prisms. Read before the American Association
of Certified Orthoptists at the 70th Annual Session of the American
Academy of Ophthalmology and Otolaryngology, Chicago, 1965 3. Jampolsky A, Flora MC, Thorson JC: Membrane Fresnel prisms: A new therapeutic
device. In Fells P (ed): Proceedings of the First Congress of the
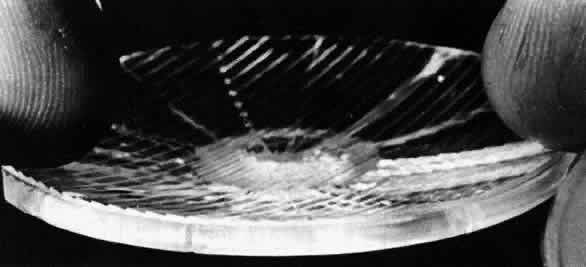
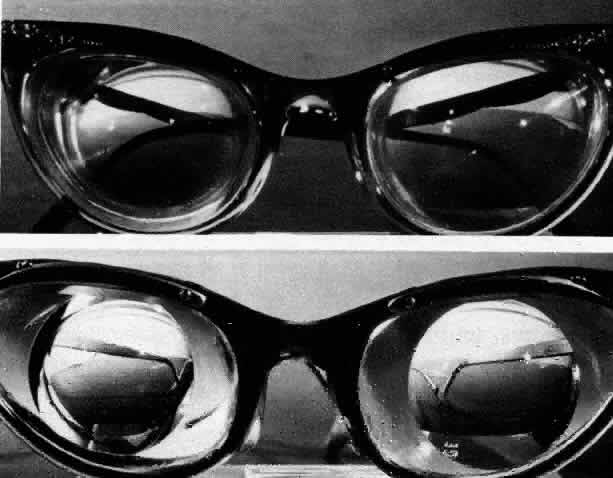
International Strabismological Association. London: Kimpton, 1971, p 183 4. Kors KK, Flora MC, Adams AJ: Fracturing and safety properties of glass spectacle lenses having back
surface vinyl membranes. Am J Optom 49:471, 1972 5. Adams AJ, Kapash RJ, Barkan E: Visual performance and optical properties of Fresnel membrane prisms. Am J Optom 48:289, 1971 6. Ogle KN: Distortion of the image by prisms. J Opt Soc Am 41: 1023, 1951 7. Ogle KN: Distortion of the image by ophthalmic prisms. Arch Ophthalmol 47:121, 1952 8. Miles PW: Eliminating distortion due to prisms in glasses. Am J Ophthalmol 34:87, 1951 9. Morgan MW: Distortions of ophthalmic prisms. Am J Optom 40:344, 1963 10. Barkan E, Kapash RJ: Visual performance and optical properties of Fresnel
membrane prisms: I. Residual astigmatism and spherical power. Read
before the Annual Meeting of American Academy of Optometry, New York, 1972 11. Wild BW: Single vision lenses. In Borish IM: Clinical Refraction, ed 3. Chicago: Professional
Press, 1970, p 1086 12. Clippers C: Comments on paper presented by Jampolsky et al. In Fells P (ed): Proceedings
of the First Congress of the International Strabismological
Association. London: Kimpton, 1971, p 190 13. Arruga A: Aplicaciones de los prismas membranosos en terapeutica estrabologica. Arch Soc Esp Oftal 31:381, 1971 14. Kapash RJ, Barkan E: Fresnel optics and human visual performance. Paper
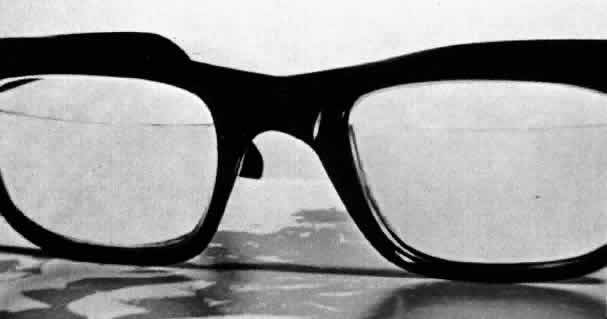
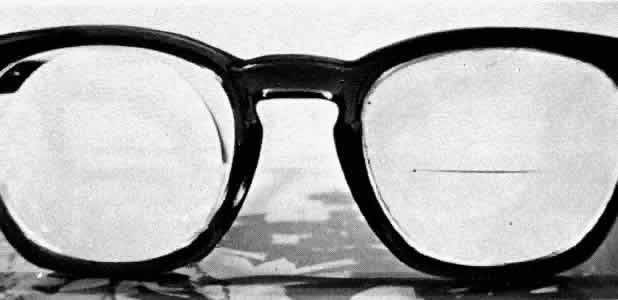
presented at the Annual Meeting of the American Academy of Optometry, Ontario, 1971 15. Miller OE, McLeod JH, Sherwood WT: Thin sheet plastic Fresnel lenses of high aperture. J Opt Soc Am 41:807, 1951 16. Hirsch M J: Prism in spectacle lenses for cosmesis. Am J Optom 45:409, 1968 17. Flom MC: Treatment of binocular anomalies of vision. In Hirsch MJ, Wick
R (eds): Vision of Children. Philadelphia: Chilton, 1963, p 197 18. Guibor G: Squint and Allied Conditions. New York: Grune & Stratton, 1959 19. Weiss NJ: An application of cemented prisms with severe field loss. Am J Optom 49:261, 1972 20. Wechsler S, Weisman B: Fresnel lenses to correct twenty-four diopters of myopia. Am J Optom 49: 1030, 1972 21. Wick B: Uses of minus Fresnel press-on(tm) lenses to improve eyewear appearance in moderate to high myopia. Am J Optom 51:343, 1974 |