| Other than the traditionally recognized bandage soft lenses, there are
other therapeutic uses for contact lenses. Some are soft lenses; many
are rigid lenses, typically rigid gas permeable (RGP) lenses. Specialty
lenses are mostly used in situations in which neither spectacles nor
a conventional lens would improve visual acuity or relieve patients from
debilitating symptoms. Some examples are keratoconus, after corneal
transplantation, irregular astigmatism of various etiologies, color
deficiency (particularly red-green), diplopia, anisometropia, cosmetically
unsightly eyes, iris abnormalities with resultant monocular diplopia, photophobia, glare, halos, or decreased vision. KERATOCONUS DESIGN LENSES Patients with keratoconus disease comprise a significant portion of the
population of therapeutic contact lens wearers (Figs. 3 and 4). Although patients with early forms of the disease may obtain reasonably
good visual acuity with either spectacles or conventional soft lenses, most
patients require special design, rigid lenses to obtain functional
vision. Eliminating the need for corneal transplantation would
be ideal. Because of the high degree of irregular astigmatism and the
nature and location of the ectasia that patients with keratoconus have, conventional
lens fitting does not provide these patients with either
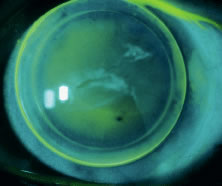
an adequate fit or reasonable comfort or visual acuity.  Fig. 3. Keratoconus. Corneal ectasia outline using retro illumination. Fig. 3. Keratoconus. Corneal ectasia outline using retro illumination.
|
 Fig. 4. Keratoconus—Munson's sign. Fig. 4. Keratoconus—Munson's sign.
|
The purpose of a contact lens in patients with keratoconus is to cover
the irregular astigmatism and the distorted anterior surface of the ectatic
cornea, thus providing a regular, spherical optical surface in front
of the eye. The lens would effectively restore the smooth optical
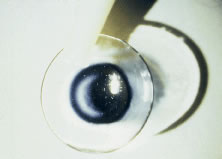
properties of the cornea (Figs. 5 and 6).  Fig. 5. Advanced keratoconus fit with Nicone RGP lens with resultant 20/25 vision. Fig. 5. Advanced keratoconus fit with Nicone RGP lens with resultant 20/25 vision.
|
 Fig. 6. Fellow eye of patient in Figure 5—after penetrating keratoplasty. Acuity without correction: 20/200 Fit
with keratoconus lens design improving visual acuity to 20/30. Fig. 6. Fellow eye of patient in Figure 5—after penetrating keratoplasty. Acuity without correction: 20/200 Fit
with keratoconus lens design improving visual acuity to 20/30.
|
There are numerous keratoconus lens designs available in the market. The
primary goal of each design is to allow adequate fitting over the diseased
cornea with minimal or no direct mechanical trauma to the normal
tissue. This is typically accomplished with designs that incorporate
several different posterior curvatures in which the central curvature
is steeper and the peripheral curves are flatter. Some lenses are bicurved, tricurved, or
even multicurved. Aspheric lenses are often used. Some of the lens designs available today for patients with keratoconus
include: - Soper Cone—bicurved
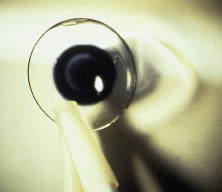
- Nicone—tricurved (Fig. 7)
- Aspheric lenses (complex)
- Mc Guire
- Rose K
- Comfort Kone
- KAS Lens
- Valley K
- Porus K
- Formacon
- Piggy-back lenses
- Softperm (hybrid)
- Scleral (haptic) lenses
- Flexlens Tricurve keratoconus lens (soft)
- Flexlens Harrison keratoconus lens (soft)
- Dura-T
 Fig. 7. Nicone lens design—for keratoconus patients. Fig. 7. Nicone lens design—for keratoconus patients.
|
Although some of these lenses may be available in PMMA hard lens material, it
is highly recommended that gas permeable materials be used to avoid
further compromise on an already diseased cornea. In the hands of an experienced contact lens fitter, most moderate and many
advanced cases of keratoconus can be successfully fitted with contact
lenses (Fig. 8). Today, a much lower percentage of keratoconus patients require corneal
transplantation, because of the technologic advances and the many contact
lens options available.  Fig. 8. Keratoconus patient successfully fit with Nicone lens. Fig. 8. Keratoconus patient successfully fit with Nicone lens.
|
IRREGULAR ASTIGMATISM Significant irregular astigmatism can result from ocular surgery, although
it is most commonly seen in patients with penetrating injuries or
in patients with significant corneal surface pathology. When the amount
and extent of the irregular astigmatism is mild, soft contact lenses
can be used successfully. When soft lenses are used, it is recommended
that a thick lens be used. The thicker lenses will allow less flexure, thus
creating an effective tear-lens layer. In most cases, a rigid lens is needed due to the large amount of irregular
astigmatism. Rigid lenses will usually provide patients with a better
visual acuity. Whenever possible, a thin, spherical gas permeable
lens is preferred. The fitting technique may vary, although care should
be given to protecting the cornea from lens trauma to the areas of protrusion (Fig. 9). Although a relatively thin lens is recommended, flexure will be a problem
if the lens selected is too thin. In patients who cannot tolerate
rigid lenses, either piggy-back lenses or a hybrid lens may be used
successfully.  Fig. 9. Advanced keratoconus fit with special design (Nicone) RGP lens. Fig. 9. Advanced keratoconus fit with special design (Nicone) RGP lens.
|
The initial lens selection may be difficult because of the inability to
obtain accurate keratometric readings. If keratometry is not possible, it
may be helpful to use keratometric readings from the fellow eye. Whenever
possible, corneal topography is recommended because it is usually
helpful in visualizing the cornea of patients with irregular astigmatism. With
the use of corneal topography combined with a computerized
lens design program, highly specialized lenses may be generated to
fit the difficult patient. PIGGY-BACK LENSES The piggy-back lens concept is basically the wearing of both a soft and
a rigid contact lens to provide the patient with the good visual acuity
of a rigid lens and the comfort of a soft lens. In the piggy-back lens
system, the patient wears a soft lens against the cornea, which provides
comfort, and a rigid lens over the soft lens to obtain good, useful
vision. Piggy-back lenses are typically used in cases of keratoconus or in patients
with irregular astigmatism after a penetrating keratoplasty or as
a result of a penetrating injury (traumatic). Standard soft lenses are applied to create a new anterior surface of the
lens/cornea combination. On the surface of the soft lens, the appropriate
RGP lens is placed. The rigid lens typically has a steep central
posterior curve surrounded by a flatter peripheral zone. The steep central
zone stabilizes on the corneal cap while the flatter zone rests
on the periphery of the soft lens. Some laboratories will create a custom
lens with an anterior depression in the soft lens in order for the
rigid lens to fit properly. This feature provides better centration because
the rigid lens fit into the shallow depression of the soft lens. The primary advantage of the piggy-back lens system is comfort. Disadvantages
include: cost, extensive patient education, and laborious care
and handling of the lenses. A possible complication is decreased oxygen
permeability, because there are two superimposed lenses over the corneal
surface. This is of particular concern in these patients because
the corneas are already diseased and/or compromised. CONTACT LENSES FOR SPORTS Generally, soft contact lenses are preferred for any contact sports or
athletics because of the danger of the rigid lens being displaced off
the cornea or even out of the eye. This has happened so frequently that
the National Basketball Association has passed a rule that games cannot
be stopped to look for a lens that accidentally pops out of a team
member's eye. Athletes often need rigid lenses to obtain the desired or needed visual
results. In these cases, a large-diameter lens must be fitted. These
large-diameter lenses can often be tolerated for only 4 to 5 hours at
a time. To provide the best possible fit with increased wearing time, lenses with
additional peripheral curves are often used. The larger diameter will
provide increased apical vaulting that requires peripheral modifications. Aspherical
lenses are best for these circumstances. These may be
available in diameters as large as 10.0 mm. Aspherical lenses offer
the following advantages: not easily dislodged; better comfort; improved
visual acuity; and less photophobia because of the better fit and larger
optical zone, therefore, they are better tolerated. Soft lenses are typically preferred for contact sports because they move
the least and are almost impossible to dislodge. Soft lenses will also
follow sudden eye movements well, thus improving performance. They
also cause less photophobia and are extremely comfortable. Wearing time
is flexible with soft lenses. Dust and foreign bodies do not usually
affect wear as is the case with rigid lenses, because dust and foreign
bodies do not become trapped underneath the lens. Whenever possible, soft
lenses are best for soccer, basketball, softball, football, tennis, rugby, cricket, lacrosse, polo, squash, racquetball, skiing, hockey, and
other contact sports. The major disadvantage of soft lenses is
that the contrast sensitivity is not quite as good as that of RGP lenses. NYSTAGMUS Patients with congenital nystagmus see poorly with glasses. The oscillations
of the eyes with spectacles produce constant parallax. With contact
lenses, the visual disturbance that is created by the constant eye
movements against a fixed spectacle is greatly reduced, thus improving
the functional vision. The visual gains for nystagmus patients can be
remarkable and can be improved from 20/200 to 20/50 or even better with
the use of contact lenses. As fixation is improved by the corrective lenses, the actual amplitude
of the oscillations may decrease. This is particularly noticeable under
dim illumination. Most patients with nystagmus seem to have a large amount of astigmatism. Properly
correcting the astigmatism is of utmost importance, particularly
when the goal is to improve the patient's overall visual acuity. Some
prefer fitting these patients with large-diameter RGP lenses, although
some of us prefer to use soft toric lenses, often custom made, with
good axis stability. The advantage of the soft lens, which is
used whenever possible, is greater axis stability with the nystagmus. Patients with albinism almost invariably have a significant nystagmus and
large amounts of astigmatism. These patients not only benefit from
contact lenses for the reasons discussed previously but also benefit from
a tinted lens to decrease the photophobia that they have as a result
of the translucent iris. Decreasing the photophobia will also enhance
their vision, as well as their comfort and functionality. ORTHOKERATOLOGY Orthokeratology is a method of correction of refractive errors using a
series of rigid contact lenses to change the shape of the cornea, thus
altering the refractive error. It is said to be a system for “sight
without glasses.” Orthokeratology has been available for many
years although its popularity has varied through the years. With the
increasing popularity of refractive surgery, orthokeratology has become
somewhat more popular. Its reversibility has made it an attractive
alternative to refractive surgery. The premise behind the system is that progressive flattening of the cornea
through the use of a series of flatter fitting lenses will eliminate
myopia. The assumption is made that the degree of flattening will be
uniform in all meridians. Certainly this is not always the case. Flat
fitting lenses worn over a long period may result in a toric cornea. The advocates of orthokeratology point to its usefulness in treating certain
groups of patients who require good vision and cannot wear contact
lenses. With orthokeratology, lenses can be applied as night lenses and removed
during the day. The night wearing maintains the flatness of the cornea (retainer
effect). Lenses must be reassessed at least every 6 weeks
with repeated attention to the refraction. New corneal readings and slit
lamp evaluation of the cornea is required. When changes in the corneal
curvature occur, new flatter lenses are provided. Often a retainer plano lens is worn, sometimes for a minimum wearing schedule, to
keep the cornea flat. Most ophthalmologists have very limited
experience with orthokeratology. Complications such as over-wear reactions, corneal abrasions, induced corneal
astigmatism, corneal warpage, and ocular discomfort from the wearing
of such a large, flat lens can occur. The main objections of orthokeratology
are (1) corneal complications from the use of overnight contact
lens wear (e.g., hypoxia, corneal edema), (2) cost and time expenditure, (3) unpredictable effectiveness and inability to screen patients
for accurate patient selection, (4) necessity of a retainer contact
lens, and (5) usefulness only in myopic patients. AFTER REFRACTIVE SURGERY As refractive surgery has become increasingly popular, the need for specialized
contact lens fitting after refractive surgery has increased significantly. There
are several uses or needs for contact lenses after
refractive surgery: (1) “molding lens” to reshape the cornea
and promote healing under the laser-assisted in-situ keratomileusis (LASIK) flap, (2) bandage—to minimize pain in cases of photoreactive
keratectomy (PRK) or in cases in which there is any abrasion occurring
with LASIK or any other refractive procedure, (3) correction of
irregular astigmatism resulting from the surgery, (4) correction of
any residual refractive error not corrected by the surgery, (5) treatment
of anisometropia in patients that have only undergone surgery in one
eye, and (6) others. Following refractive surgery, patients usually have a very different and
distinct corneal anatomy that often makes lens fitting difficult. This
is especially the case with patients who have undergone RK and similar
procedures. Their corneal anatomy is quite different than that of
nonsurgical patients. New lens designs, particularly rigid lenses, have been developed to fit
these patients. Similar to postkeratoplasty patients, the corneas of
these patients have a flat central area surrounded by a steeper periphery. Conventional
lenses cannot be successfully fit in most of these patients. POSTTRAUMATIC Patients who suffer penetrating injuries to the eye often need or benefit
from contact lenses. As mentioned earlier, the correction of irregular
astigmatism is best accomplished with the use of a rigid lens. Irregular
astigmatism cannot usually be corrected with either spectacles
or soft lenses. Most patients with penetrating injuries have resultant
irregular astigmatism. Large ametropias often require contact lenses to avoid anisoconia and diplopia
and to achieve functional visual acuity. Monocular aphakia is
a common complication of trauma. Restoration of vision is accomplished
with the use of a contact lens whenever intraocular lens implantation
is not feasible or contraindicated. Posttraumatic iris abnormalities are another common complication after
penetrating trauma: traumatic mydriasis and traumatic partial or total
aniridia. These abnormalities are often best corrected with the use of
an iris-painted soft contact lens. Lens use in these cases can be beneficial
both cosmetically and functionally. Cosmetically, covering an
unsightly eye can help the patient recover emotionally and can improve
the self-esteem. Functionally, correcting the iris anomalies can eliminate glare, flare, halos, and
monocular diplopia. Strabismic abnormalities often develop
after trauma that will often cause diplopia. A black pupil lens can offer
occlusion that will eliminate the diplopia. Thorough evaluation of a posttraumatic patient can identify problems and
deficiencies that are often treatable with the use of a contact lens. Combinations
can be custom made to treat these patients. OCCLUSION THERAPY Amblyopia and diplopia are the two primary indications for occlusion therapy. Occlusion
therapy has been most commonly done with patches, but
contact lenses are a more palatable, cosmetically acceptable option for
many patients (Figs. 10 and 11). 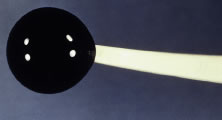 Fig. 10. Occluder (soft) contact lens. Fig. 10. Occluder (soft) contact lens.
|
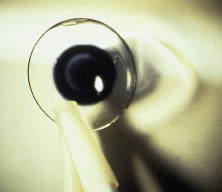 Fig. 11. Soft occluder lens—clear periphery with black pupil only. Fig. 11. Soft occluder lens—clear periphery with black pupil only.
|
The use of occluder lenses in children for the treatment of amblyopia has
been somewhat controversial. Conservatives believe that the risks of
a contact lens outweigh their benefits. Concerns about infections are
the main focus of this controversy. Another concern is hypoxia and the
complications associated with extended wear because these very young
patients do spend a significant percentage of their days sleeping. They
are not often used but, whenever used, they are usually quite successful. Contact lenses are a very successful tool in the treatment of diplopia, both
monocular and binocular. Strabismus, neurologic disorders, and trauma
are the most common causes of diplopia. In most cases the diplopia
is binocular, although, in trauma cases monocular diplopia associated
with iris anomalies is not uncommon. Patients with diplopia are often
quite debilitated with the symptoms, and the relief offered by the
lenses is usually quite welcome. Depending on the anatomy of the eye, these lenses can be either an occluder (black-out) lens
or a simple black pupil lens. The traditional black-out
lens is a soft lens that is painted black and totally opaque on
its entire surface. Although successful in providing coverage of the
visual axis, thus relieving the symptoms, it is not cosmetically appealing, especially
in patients with light colored eyes. The most commonly
used type of lens is a clear soft contact lens with a black pupil in
the center. The pupillary diameter will vary depending on the patient's
pupil diameter and positioning of the eye. Careful attention
must be paid to the position of the eye to avoid allowing light and vision
through the periphery of the painted pupil. In many cases it is necessary
to enhance the occluder effect of the lens, because patients
can still see through the lens, and thus symptoms are not eliminated. A
technique that can be used with great success is the use of a contact
lens with a power that is completely different than the patient's
refractive error. This lens (power) will provide some significant blurring
of the vision that, together with the blocking effect of the black
pupil, will in fact obstruct the vision. Although some patients report
some vision out of the eye with the lens, most are able to learn
to suppress the image in the covered eye enough to obtain symptom relief. In patients with monocular diplopia, the symptoms are caused by iris abnormalities
that in effect create two different visual axis. In most cases
the iris abnormalities are traumatic, although they can be iatrogenic (as
in patients with peripheral iridectomies that are not covered
by the eyelids). Although rare, monocular “multiplopia” can
occur. This is usually seen in trauma patients or in patients that
have undergone multiple intraocular surgeries and have several iridectomies
that are not covered by the eyelids. In patients with monocular diplopia, the type of occluder lens needed is
usually different, because the goal of therapy in these patients is
to create a single pupil. These patients typically require an opaque iris-painted
lens that will cover the entire iris and creates a single, central, clear
pupil. These types of lenses are usually more complex
to fit but are usually quite successful. COLOR DEFICIENCIES Approximately 8% to 10% of males and 0.5% of females have some impairment
in color vision ranging from a mild deficiency to an almost complete
impairment. The defect is most commonly in the red-green range. Although
yellow-blue deficiencies are seen, they are much less common. The X-Chrom lens can be used successfully to treat these patients (Fig. 12). The X-Chrom lens transmits light in the red zone from 590 to 700 nm (spectrum
of white light is 380 to 760 nm), thus improving color discrimination
in patients with partial impairment in the red-green range. The
lens is bright red, usually rigid, and fitted to the nondominant eye. The
other eye either remains uncovered or is fitted with a conventional
lens for the correction of any ametropias that the patient might
have (the X-Chrom lens can be obtained in any power, so that it can also
correct any refractive error). The uncovered eye will perceive a red-green
object as usual, but the eye with the red lens will perceive
the red wavelengths of light and will absorb the green wavelengths. The
brain now receives two different intensities. By a rapid self-learning
process, the patient can identify both colors properly.  Fig. 12. X-Chrom lens (bright red rigid lens) for red-green color deficiency. Fig. 12. X-Chrom lens (bright red rigid lens) for red-green color deficiency.
|
We have significant experience with this lens with reasonably good results. Although
the lens does not correct the color defect, it does permit
patients to make a discriminatory judgment of color. During the initial
patient evaluation, it is very helpful to use a trial lens to evaluate
effectiveness. Patients can often improve their results in the Ishihara
plates from properly identifying 1/15 plates to identifying 10/15 to 13/15 correct
plates. Proper color discrimination is very important
in numerous professions such as: electrical engineers, uniformed
forces, artists, painters, printers, decorators, and all those professions
in which color discrimination is important. A word of caution to patients wearing the X-Chrom lens: This lens has detrimental
effects on space localization of moving objects and other aspects
of binocular vision. Persons operating moving vehicles wearing
a tinted lens over one eye may experience hazardous distortions of the
positions of perceived objects and may, therefore, be dangerous drivers
in certain circumstances. Conservative judgments are justified until
the extent of the hazards is better understood. Ideal lens fitting involves special attention to avoiding excessive lens
movement and decreasing lens thickness to improve visual results. Otherwise, techniques
used for fitting any other conventional rigid lens
should be applied. Motivation is quite important because the lens may
be cosmetically undesirable (bright red lens in only one eye) and there
is an adaptation period that the patients must undergo. The use of
bright ambient light is highly recommended to maximize results. THERAPEUTIC USES OF PAINTED LENSES Painted contact lenses have a variety of uses: cosmetic, therapeutic, handling, and
informational. Although a valuable tool in total patient
care, the therapeutic use of tinted lenses is, unfortunately, not often
considered. There are several basic categories or types of painted lenses that can
be obtained, considering that multiple variables can be incorporated into
any of these lenses. As a general rule, soft (hydrophilic) lenses
are used for painting in therapeutic lenses (although rigid lenses may
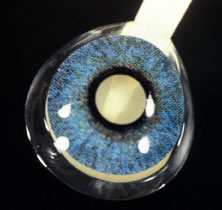
be used rarely). The broad categories of tints include: translucent (Fig. 13); opaque (iris) (Fig. 14), with or without pupillary opening; clear or black pupil; clear lens
with black pupil only (Fig. 15), totally black (occluder) (Fig. 16) lens, and others. Although some lenses are commercially available (with
predetermined colors and options), others are custom made for each
patient. The type of lens chosen for each patient will be dictated by
the patient's needs and desires. As a general rule, custom made lenses
will be more costly and take longer to obtain but usually accomplish
a better cosmetic result and, therefore, greater success. Painted
lenses can be obtained with or without refractive power, depending on
the patient's needs.  Fig. 13. Translucent iris-painted lens with black pupil. Fig. 13. Translucent iris-painted lens with black pupil.
|
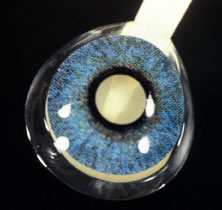 Fig. 14. Opaque iris-painted lens with clear pupil. Fig. 14. Opaque iris-painted lens with clear pupil.
|
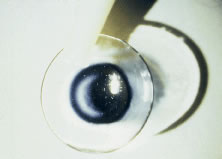 Fig. 15. Clear lens with black pupil. Fig. 15. Clear lens with black pupil.
|
 Fig. 16. Opaque black lens (occluder). Fig. 16. Opaque black lens (occluder).
|
Indications for the use of therapeutic painted lenses include: covering
corneal scars, creation of a pupil, pupillary occlusion, diplopia, heterochromia, phthisis, amblyopia, aniridia, and photophobia. While evaluating a patient for a painted lens, we must take into consideration
not only the obvious cosmetic or clinical deformities but also
the patient's realistic needs, desires, and expectations. It could
be quite frustrating if unrealistic expectations are set or the patient's
needs are not met. - Covering corneal scars—pathologic or traumatic, (Figs. 17 and 18) severe corneal neovascularization, aphakic bullous keratopathy, infections, penetrating
injuries, and phthisis. In these cases, an iris-painted
lens with a black pupil is needed. Occasionally a clear pupil may
be necessary if the eye has functional vision. The iris may be covered
with a dark brown translucent lens if the iris in the counter eye is
very dark brown as well. Otherwise, an opaque iris lens may be necessary.
- Creation of a pupil—traumatic or surgical. Pupillary defects are
most commonly seen as a result of trauma (blunt or penetrating), although
surgically induced defects can often be seen as well, for example: removal
of iris tumors (Fig. 19), intra-operative difficulties, anisocoria, and others. For these cases, opaque
iris-painted lenses with a clear pupillary opening are usually
necessary.
- Occlusion of pupil—amblyopia, leukocoria (Figs. 20 and 21). The condition may be cosmetic or therapeutic. For the treatment of amblyopia
in a child, an opaque black lens may be used. Cosmetically, patients
with leukocoria may also benefit from a similar lens.
- Diplopia—monocular or binocular. Diplopia may occur in patients with
neurologic disorders, acquired strabismus, and others. Monocular diplopia
may be seen in patients with traumatic or surgically induced peripheral
iridectomies that are within the interpalpebral fissure. There
may be other causes. A lens with a painted black pupil, with or without
a painted iris, may be quite successful.
- Heterochromia—congenital or acquired. Patients who have heterochromia
are often very self-conscious of their cosmetic appearance. This
may be corrected with the use of an opaque iris-painted lens colored to
match the opposite eye. This is usually done to match the darker eye. Occasionally, lenses
may need to be used in both eyes to obtain a good
cosmetic result.
- Phthisis—unsightly, blind eye. The significant social, cosmetic, and
psychologic effects from a phthisical eye can be devastating to some
patients. With the use of a painted lens, these patients can resume
normal lifestyles. An opaque iris-painted lens with a black pupil offers
the best results. Iris color and diameter are selected to best match
the fellow eye.
- Amblyopia—therapeutic. Amblyopia therapy often fails only because
of the parent's inability to maintain the patch over the child's
eye. An occluder contact lens may be very successful because the
child is unable to remove the lens or “peek around it.” Psychologically, this
alternative can also be very advantageous.
- Aniridia and albinism—surgical or traumatic partial or total aniridia (Figs. 22 and 23). Patients with partial or total aniridia (congenital or acquired, surgical
or traumatic) may greatly benefit from an opaque iris-painted lens. If
the eye is sighted, a clear pupil is used, and the lens may also
have the refractive power incorporated into the lens for visual correction. A
clear lens may be used in the opposite eye if necessary and
so desired. In other cases, it may be necessary to have a black pupil
of the desired diameter to match the other eye.
Patients with albinism have often benefited from tinted lenses. The lenses
are used to decrease the photophobia caused by the iris transillumination. Some
patients need only a translucent lens whereas others require
an opaque iris-painted lens because of their severe photophobic symptoms. In
some patients (psychologic reasons) cosmesis is an important
factor to address.
- Photophobia—normal eyes that are abnormally light sensitive. These
patients, as well as individuals with pupillary abnormalities, corneal
pathology, and other anterior segment anomalies, also benefit from
tinted lenses.
As we review the numerous uses of contact lenses, cosmetic as well as therapeutic, rigid
and soft, we realize that contact lenses should always
be regarded as an integral part of all ophthalmologist's armamentarium
for total patient care. We should consider contact lenses not
just as a means to eliminate spectacle correction but also as a medical
device that can greatly improve quality of vision and quality of life. The
therapeutic uses of contact lenses are numerous and varied. It
is extremely rewarding, to both the patient and the ophthalmologist, to
be able to improve the quality of life of those patients we fit with
any of the specialty lenses.
 Fig. 17. Posttrauma patient with resultant cosmetically unacceptable corneal scars. Fig. 17. Posttrauma patient with resultant cosmetically unacceptable corneal scars.
|
 Fig. 18. Patient in Figure 17 fit with a soft, translucent iris-painted lens and black pupil. Fig. 18. Patient in Figure 17 fit with a soft, translucent iris-painted lens and black pupil.
|
 Fig. 19. Young girl with iris melanoma surgically removed with resultant surgical
aniridia. Patient severely photophobic and self-conscious of cosmetic
appearance. Patient was successfully fit with an opaque iris-painted
lens with a clear pupil. Fig. 19. Young girl with iris melanoma surgically removed with resultant surgical
aniridia. Patient severely photophobic and self-conscious of cosmetic
appearance. Patient was successfully fit with an opaque iris-painted
lens with a clear pupil.
|
 Fig. 20. Patient with traumatic cataract and total retinal detachment (leukocoria) resulting
from severe trauma. Fig. 20. Patient with traumatic cataract and total retinal detachment (leukocoria) resulting
from severe trauma.
|
 Fig. 21. Patient from Figure 20 after fitting with very dark, translucent iris-painted lens with black
pupil. Fig. 21. Patient from Figure 20 after fitting with very dark, translucent iris-painted lens with black
pupil.
|
 Fig. 22. Patient with traumatic aniridia (hockey puck injury) resulting in severely
photophobia and a cosmetically unacceptable eye. Fig. 22. Patient with traumatic aniridia (hockey puck injury) resulting in severely
photophobia and a cosmetically unacceptable eye.
|
 Fig. 23. Patient from Figure 22 after fitting with a rigid, opaque iris-painted lens with clear pupil. Fig. 23. Patient from Figure 22 after fitting with a rigid, opaque iris-painted lens with clear pupil.
|
|