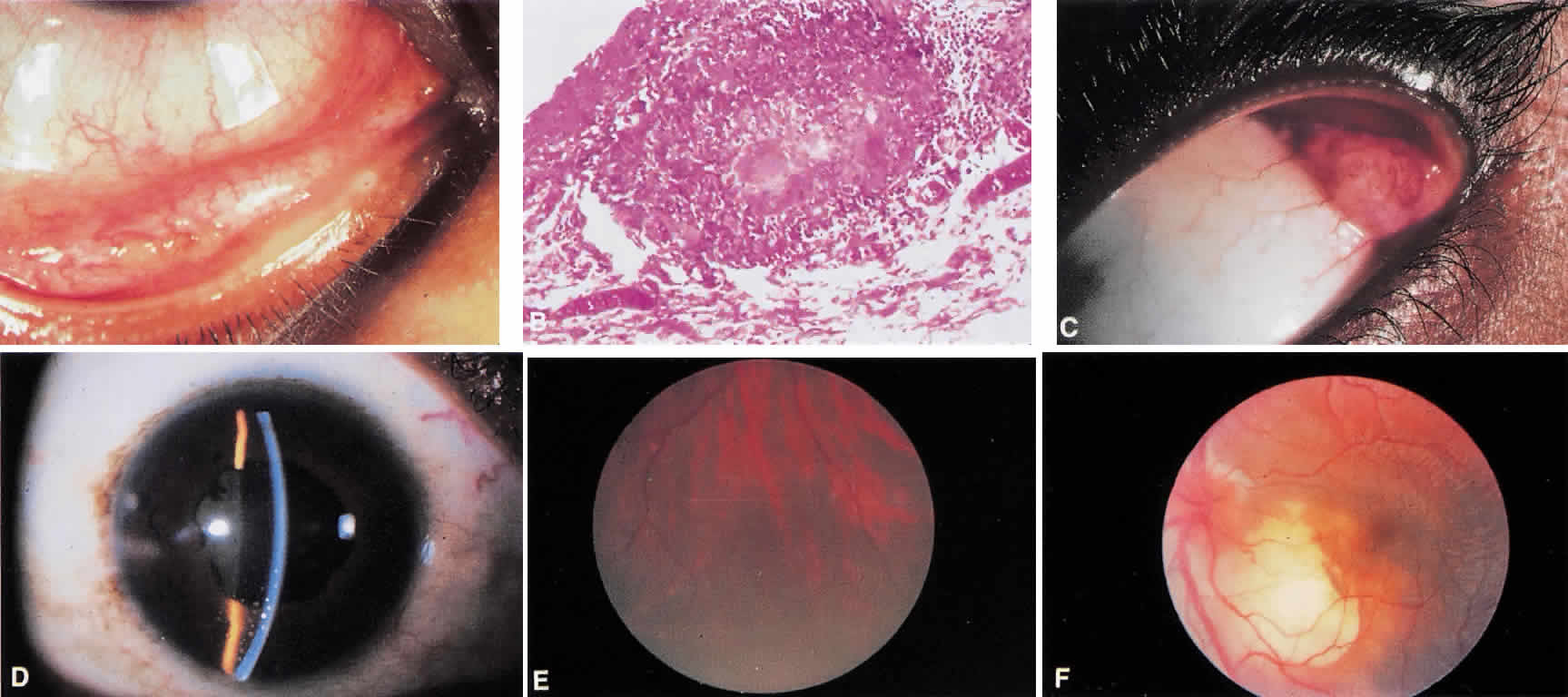
Lacrimal gland enlargement (see Fig. 1C) or dacryoadenitis may be an early finding in sarcoidosis, but it is the initial manifestation of the disease in approximately 1% of patients.9 The differential diagnosis of lacrimal gland enlargement is listed in Table 2. A biopsy demonstrating noncaseating granulomas can differentiate lacrimal gland enlargement caused by sarcoidosis.
TABLE 2. Differential Diagnosis of Lacrimal Gland Enlargement
Sjögren's syndrome
Sarcoidosis
Lymphoma
Leukemia
Systemic lupus erythematosus
Wegener's granulmatosis
Amyloidosis
Other connective tissue disease
Corneal sarcoidosis may be either interstitial keratitis or localized stromal opacification secondary to endothelial decompensation in areas where keratic precipitates once were present.10 Neither type of corneal involvement is specific for sarcoidosis. The sclera may rarely be a site of activity in sarcoidosis. Granulomatous scleritis is a localized form of nodular scleritis, which may be seen in sarcoidosis, and posterior scleritis has been reported in sarcoidosis.11
Uveitis in sarcoidosis may be granulomatous or nongranulomatous, acute or chronic, localized or diffuse, and monocular or bilateral. However, anterior uveitis is the most frequent type of uveitis seen in patients with sarcoidosis. Either acute or chronic iridocyclitis may occur. Acute iritis presents most often in women, between ages 20 and 30, with pain, redness, and photophobia. There is generally moderate anterior chamber flare and cells, and keratic precipitates are usually small or fine. The presence of large keratic precipitates is suggestive of inflammation of long duration, but may be seen acutely. (see Fig. 1D). Large or mutton-fat keratic precipitates are not specific for sarcoidosis. Iris nodules on the pupillary border (Koeppe nodules) or in the midstroma (Busacca nodules) may be present. Vitreous cells are frequently present, and when accompanied by anterior chamber reaction, without posterior involvement, the condition is called iridocyclitis. Acute sarcoid iridocyclitis does occur. Visual acuity may be normal, but with associated cystoid macular edema, it may decrease. Acute iridocyclitis may be unilateral or bilateral.
Chronic iridocyclitis in sarcoidosis is frequently associated with cystoid macular edema. Patients with this condition may not have pain or redness, but they present with blurred vision and floating spots. These patients tend to be older (35 to 50 years of age) than those presenting with acute iritis.12 Keratic precipitates, either small or large, moderate anterior chamber cell and flare, posterior and anterior synechiae, and vitreous cells may all be present. Fluorescein angiographic evidence of cystoid macular edema is to be expected if visual acuity is decreased. Activity in chronic iridocyclitis in sarcoidosis tends to be bilateral.
Posterior segment intraocular inflammation frequently is present in sarcoidosis. Vitreous cellular reaction may range from minimal with few vitreous cells or clumps of cells, vitreous snowballs, to the more unusual presentation of dense vitreous debris. Histologically vitreous snowballs contain epithelioid cells.13 Retinal periphlebitis occurring in the midperiphery of the retina is highly suggestive of sarcoidosis. Small exudates near retinal veins, termed candle wax drippings may be present (see Fig. 1E). Neovascularization may occur. Choroidal granulomas may be small and multiple, resembling Dalen-Fuchs nodules, or single and very large, resembling a choroidal tumor, as seen in Figure 1F. Chronic cystoid macular edema may cause decreased vision in patients with long-standing sarcoid uveitis. The optic nerve may be involved with disc neovascularization, disc edema in chronic inflammation, or with granuloma formation within the optic nerve.