A peculiar syndrome secondary to trauma, usually of the perforating type that involves the lens, is pseudoretinitis pigmentosa. There is a selective loss of the photoreceptor layer,18 extinguished electroretinogram, and migration of pigment into the retina. These features may develop within a few days after the injury.
FOREIGN BODIES
Rarely, localized choroiditis is associated with penetrating intraocular foreign bodies as an isolated feature. The condition of the host, the manner of penetration, and the character of the foreign body must have been so correlated as to avoid the more devastating endophthalmitis. Relatively inert foreign material (e.g., glass, stone, quartz) may lodge in the retina and choroid and cause a low-grade inflammatory response that walls off the foreign substance. Such an inflammation may simulate other types of uveitis such as pars planitis and a Toxocara granuloma. A long quiescent period or intermittent recurrences of inflammatory signs may ensue. When a foreign body is nonmagnetic, systemic and periocular administration of steroids should be initiated and used in the follow-up treatment. Removal of a magnetic foreign body may be well tolerated in the choroid; its path through the eye often provokes vitreous damage and secondary retinal complications.
RETINAL PERFORATION DURING SURGICAL MANAGEMENT OF STRABISMUS
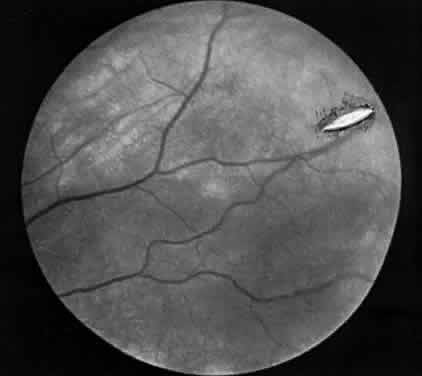
Hemorrhage initially covers the perforation site. Some of this hemorrhage may break through into the vitreous cavity but usually remains confined to the choroid and retina. In a day or two, bare sclera becomes visible, usually surrounded by residual hemorrhage and a rim of light pigmentation.19 It appears as if the choroid and the retina were scooped out, leaving bare sclera behind (Fig. 1). Inverted cutting needles seem responsible since this is a complication almost unheard of before or after their common use. Prophylaxis indicates the use of a needle that is not sharp on the convex curve. The management of these perforations remains controversial.20 In our experience, widely dilating the pupil permits nearly immediate diagnosis as the area can be clearly seen through the usually clear media. Depending on the characteristics of the perforation, transpupillary laser coagulation or direct cryotherapy can be administered easily. Some suggest, however, that observation without treatment is all that is required since the perforations are almost always self-sealing and result in no significant sequelae. Nevertheless, in a series of 728 patients with known scleral perforations, 14 (2%) of the cases had a retinal detachment and eight resolved without complications.21
|