In a series of 2111 eyes that underwent penetrating keratoplasty at L.V. Prasad Eye Institute in Hyderabad, India, corneal opacification was due to corneal scars (23.2%), aphakic and pseudophakic corneal edema (23.0%), regrafts (17.2%), active infectious keratitis (16.0%), corneal dystrophies (7.9%), keratoconus (5.5%), and various other causes (6.2%)2 (Fig. 1).
|
INFECTIONS
A variety of microbial agents cause corneal stromal degradation with consequent scarring. Of the infectious diseases, trachoma continues to be the leading cause of corneal blindness in the world. According to the WHO, almost 6 to 9 million people are blind from trachoma and more than 500 million people inhabit areas endemic to blinding trachoma. The cornea is affected secondarily to chronic progressive conjunctival pathology; blindness usually ensues after 50 years of age.
Corneal infections caused by bacteria, fungi, viruses, and parasites are a frequent occurrence in most developing countries. Poverty, illiteracy, ignorance, inaccessibility to medical care, delayed or incorrect diagnosis, nonavailability of appropriate drugs, and exposure to harmful treatment practices are impediments to effective prevention of corneal blindness. Medical attention is often sought at an advanced stage. It is not uncommon to find a large segment of eye beds occupied by patients with infectious keratitis.
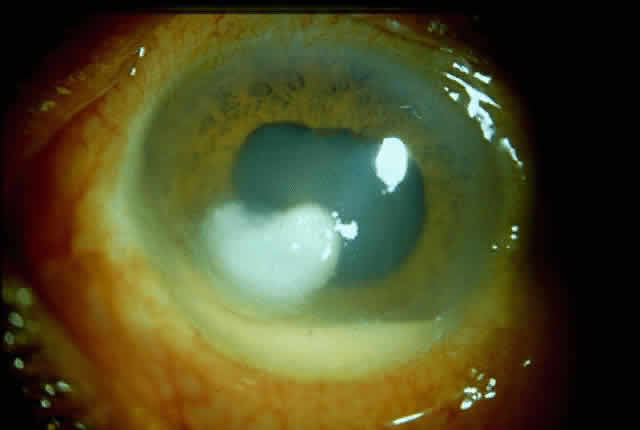
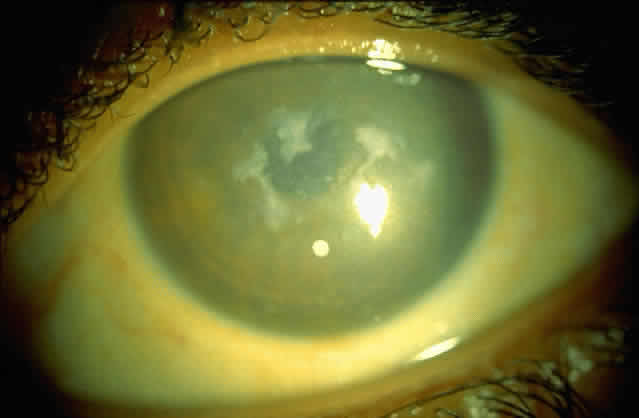
Bacterial corneal infections are caused by a wide variety of organisms. Pneumococcus seems to be the most common causative organism (Fig. 2); however, staphylococcal, pseudomonal, and gonococcal infections frequently are encountered.3 This may be related to chronic dacryocystitis.5
|
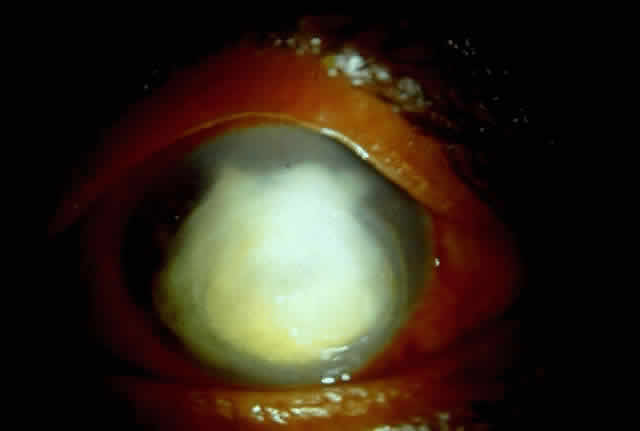
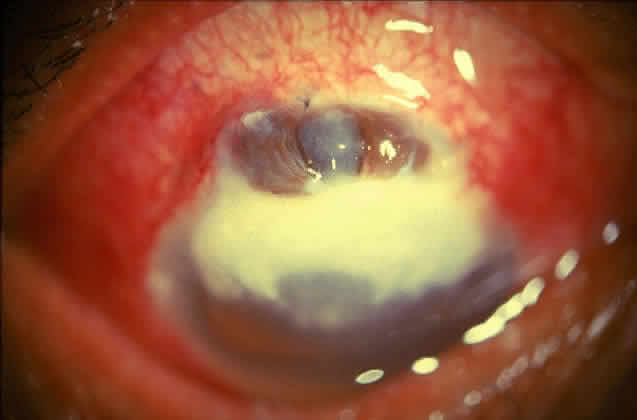
Fungal keratitis is as frequently seen as bacterial keratitis. Aspergillus and Fusarium are the two most commonly isolated organisms. Predisposing factors include trauma, foreign body, and injudicious usage of topical steroids or other indigenous medications.
Delay in diagnosis, the relative ineffectiveness of antifungal agents in most parts of the world, and the nonavailability of these drugs hinder prevention and management (Fig. 3).
|
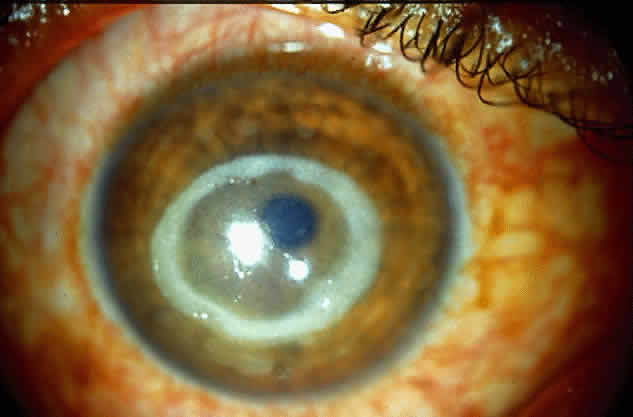
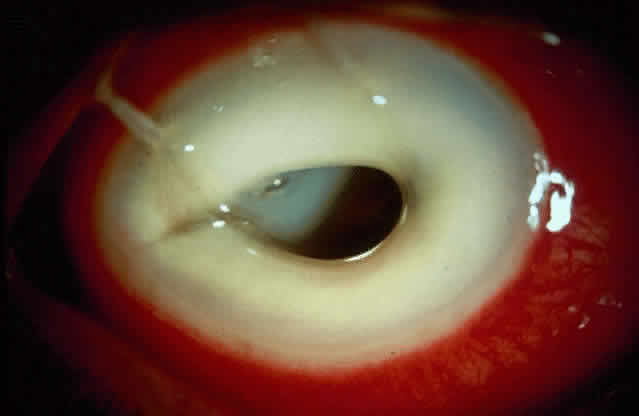
Acanthamoeba infection of the cornea is being reported with increasing frequency. While this is associated with contact lens wear in industrialized countries, in developing countries it is almost exclusively seen in non-contact lens wearers (Fig. 4).6 Misdiagnosis and inappropriate treatment are common.
|
Herpes simplex keratitis has the potential for corneal devastation, particularly when it presents as stromal disease. Failure to make the clinical diagnosis, lack of laboratory facilities, and inappropriate treatment often lead to recalcitrant stromal disease and consequent corneal opacification.
Ophthalmia neonatorum is being reported with increasing frequency.7 Absence of proper prenatal screening for venereal disease and low utilization of Crede's prophylaxis are responsible. The emergence of penicillin-producing strains of gonorrhea is yet another problematic factor.
Ocular Leprosy
As many as 10 to 12 million people worldwide suffer from leprosy, and about 250,000 million are blind from ocular leprosy.8 Involvement of the eye in leprosy has been reported from a variety of corneal manifestations, some of which may lead to blindness.9 Lagophthalmos with exposure keratitis and consequent infection resulting in scarring is an important mechanism. Hypoesthesia of cornea can also can lead to corneal ulceration and ultimate opacity.10
Onchocerciasis
Microfilariae, dead or alive, in the corneal stroma, produce “snowflake” or onchocercal punctate keratitis. Onchocerciasis can be a mild and reversible phenomenon, but severe longstanding invasion of numerous microfilariae into the cornea may lead to sclerosing keratitis, especially along the lower limbus, gradually spreading to the central optical zone.11 Sclerosing keratitis is usually seen in severe cases and is claimed to be the most common pathway to blindness in the savannas.
According to a WHO report on corneal blindness,3 nine main “ecological and behavioral niches” promote corneal ulceration through a consequence of risk factors, one of which is often infectious in origin. Adequate prevention and treatment measures include the following, which are listed according to patient or environmental characteristics:
- Newborn babies: Prevention of gonococcal ophthalmia in newborn babies by ocular prophylaxis
at birth with tetracycline ointment, improved prenatal screening, and
control of sexually transmitted diseases
- Children: In children 6 months to 6 years, especially those 1 to 3 years of age, immunization
against measles, sound weaning practices to improve sanitation, and
oral vitamin A supplements to prevent serophthamla (particularly
in cases of malnutrition), malabsorption (prolonged diarrhea), measles, or
corneal ulcers of unknown cause
- Measles epidemic: During an epidemic of measles, the prevention of overcrowding of children
and removal of contact cases, vitamin A supplementation, eye ointment, and
immediate treatment for corneal ulcers is essential
- Famine and disasters: In famine and disasters, displaced persons should receive immunization
against measles, vitamin A supplementation, and immediate treatment of
corneal ulcers
- Arid, crowded, or tropical rural areas: In these areas, where trachoma and communicable ophthalmia are predominant, prevention
and management include prophylaxis against injuries and
control of trachoma.
- Lush, humid, tropical areas and industrial settings: In these areas, prevention of and first aid for injuries is essential, particularly
corneal trauma from agricultural products that frequently
cause secondary (often fungal) infections
In East Africa between 1% and 4% of children with measles develop corneal ulcers, and almost half (46%) of unilateral and more than three quarters (79%) of bilateral corneal ulcers occur within 3 months of onset of rash. Vitamin A deficiency was the cause of 50% of these cases and 55% of cases of bilateral corneal ulcers.12 Use of local remedies and herbs were the other major etiologic causes of potentially preventable blindness.
The causes of bilateral blindness in children in Tanzania were reported to be as follows13:
Vitamin A deficiency: 45%
Harmful eye practices: 15%
Herpes simplex virus: 5%
Ophthalmia neonatorum: 5%
Cataract, uveitis, and others: 30%
Again, 40% to 50% of all cases of childhood blindness were associated with measles.