Thorough knowledge of eyelid anatomy is essential for the appreciation of the etiology and surgical intervention of lower eyelid abnormalities. The eyelid can be conceptionalized to consist of an anterior and posterior lamella. The anterior lamella consists of the skin and orbicularis muscle. The thin delicate skin of the eyelid lacks the connective tissue, fat, and pilosebaceous apparatus of the dermis that would reduce eyelid mobility. The orbicularis muscle is categorized as either orbital or palpebral portions based on its association with adjacent anatomic structures. The orbital orbicularis muscle overlies the orbital rim. The palpebral orbicularis muscle is further classified as preseptal or pretarsal based on the proximity of orbital septum or tarsus, respectively. At the eyelid margin a strip of orbicularis muscle, the muscle of Riolan, is directly associated with the eyelashes. This is responsible for the darker coloration of the slightly depressed midsection of the lid margin commonly referred to as the gray line.1
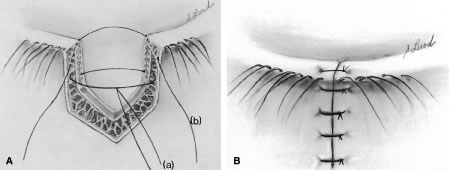
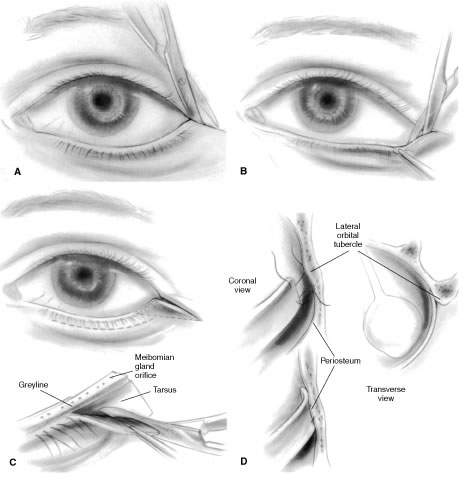
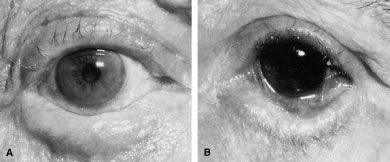
The posterior lamella consists of the eyelid retractor, the tarsus, and the conjunctiva. Hawes and Dortzbach2 reviewed and highlighted lower eyelid anatomy, specifically the lower eyelid retractor (Fig. 1). The lower eyelid is analogous to the upper eyelid; the main variation is the eyelid retractor system. The upper eyelid has a distinct eyelid retractor, the levator muscle, to enhance upper eyelid mobility. The lower eyelid does not have a specialized eyelid retractor. The lower eyelid retractor system originates as a fascial extension of the inferior rectus muscle (capsulopalpebral head). This fascial system splits to encapsulate the inferior oblique muscle and then reunites to form a dense fibrous sheet (capsulopalpebral fascia) to insert onto the inferior tarsal border. The inferior tarsal muscle is a smooth muscle analogous to the superior tarsal muscle (Müller's muscle) of the upper eyelid. This muscle originates in the inferior fornical area and extends toward the inferior tarsal border but does not insert on the tarsal border as its counterpart in the upper eyelid does. The inferior tarsal muscle receives sympathetic innervation, and interruption of its innervation will result in a slightly elevated position of the lower eyelid margin as observed in Horner's syndrome. Otherwise, the inferior tarsal muscle has little pathologic significance.
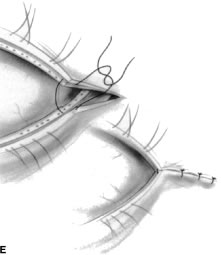
The tarsus provides the primary support or foundation for the eyelids. Although degeneration of the tarsus may promote eyelid laxity,3 the principle focus of weakness of the eyelids is at the lateral and medial canthal tendons.4 Jones and Wobig5 described the medial canthal tendon with a prominent anterior component firmly connecting the medial canthal angle to the maxillary process of the frontal bone. The posterior limb of the medial canthal tendon provides deep support to the posterior lacrimal crest. Anderson6 also emphasized the role of a superior branch of the medial canthal tendon to support the canthal angle. Gioia and coworkers7 have provided a clear description of lateral canthal anatomy. The lateral canthal tendon has contributions from the lateral aspects of the tarsus and the preseptal and pretarsal orbicularis muscle; these insert on the inner aspect of the lateral orbital rim at Whitnall's (lateral orbital) tubercle. The posterior deep insertion of the lateral canthal tendon allows the lateral aspect of the eyelids to approximate the globe.
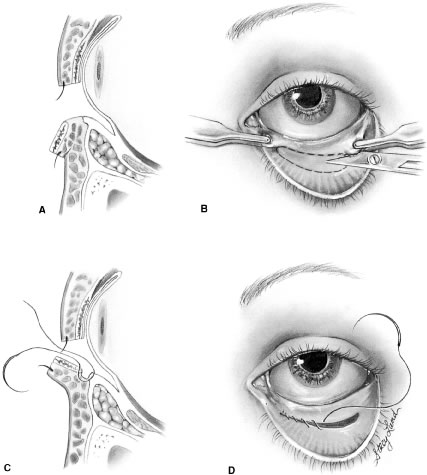
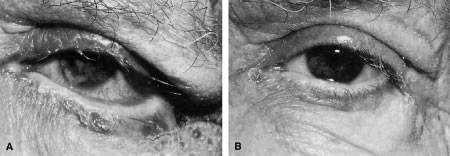
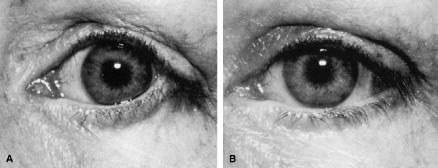
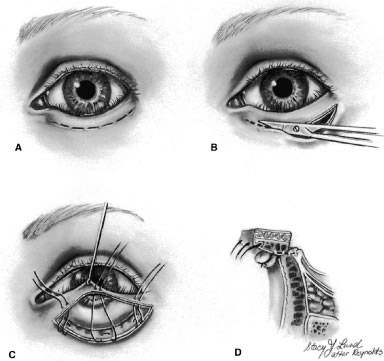
Ectropion and entropion share similar anatomic features. The most common predisposing anatomic factors for lower lid malpositions are horizontal eyelid laxity and weakness or defects of the lower lid retractors. The general weakness of the eyelid is caused by a weakness of the medial and lateral canthal tendons, permitting horizontal eyelid laxity.4 As such, it is best to consider lower eyelid laxity as resulting from laxity of the tarsoligamentous sling or support for the eyelid. The anatomic weakness can be demonstrated by the snap test. Downward retraction is exerted on the lower lid, pulling it away from the globe. On relapse, the lower lid should snap back against the globe spontaneously. Failure of the eyelid to snap back against the globe with a single blink indicates excessive laxity of the tarsoligamentous sling.
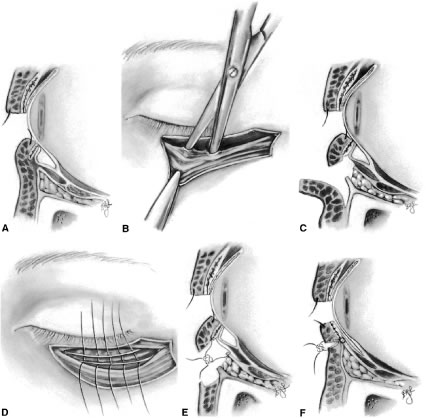
The lower eyelid retractors may be weakened or may actually become disinserted from the inferior tarsal border. Weakness or defect of the lower eyelid retractors creates in an instability of the inferior tarsal border that is manifested clinically as ectropion or entropion.
In addition, enophthalmos is associated with both ectropion and entropion. However, the role of enophthalmos as a pathophysiologic feature of lower eyelid malpositions has been grossly overstated.8,9 Enophthalmos may secondarily reduce tarsal stability by exaggerating horizontal lid laxity. It reduces the tension exerted on the eyelids by retraction of the globe and soft tissues. The normal arc or outward bowing of the eyelids is minimized with the enophthalmic globe, and eyelid tension is reduced. Retrobulbar injections stabilize eyelid malpositions by reducing horizontal eyelid laxity. Volume introduced in the retrobulbar area re-establishes the normal outward arch, or bowing, of the eyelid.
The development of ectropion and entropion is a reflection of the relationship between the anterior and the posterior lamellae. The eyelid position is maintained by an appropriate balance of the anterior and posterior lamellae. If tractional forces are unbalanced, eyelid malpositions may manifest as ectropion, entropion, or eyelid retraction. If traction is produced by the anterior lamella, either by chronic cicatricial changes or mechanical aberrations, the eyelid margin is everted away from the globe. This most commonly results from mild solar-induced changes or following surgical procedures or trauma of the eyelid, which produce a shortening or scarring of the skin and underlying orbicularis muscle.
Involutional entropion is more complex because of the multitude of factors producing this abnormality. The tarsal instability of entropic lids is due to horizontal eyelid laxity and loss of support of the lower eyelid retractors.10 The orbicularis muscle dynamics also assume a prominent pathophysiologic role in the production of entropion. In entropic eyelids, the preseptal orbicularis muscle overrides the pretarsal orbicularis muscle, which rolls the superior border of the tarsus internally. This is differentiated from spastic entropion, which is theoretically due to a spasm of Riolan's muscle. However, the primary differentiating feature of spastic entropion is a specific precipitating etiologic factor, such as recent eye surgery, eyelid edema, or ocular inflammation with secondary eyelid edema. An appreciation of the multiple etiologic causes of entropion has resulted in the evolution of combined approaches to correcting the various anatomic abnormalities and stabilizing the tarsus and orbicularis muscle.11–14
This chapter is divided into three sections that discuss eyelid abnormalities. These include ectropion, entropion, and trichiasis. Sections on ectropion and entropion are further divided according to the underlying etiology of the eyelid malposition. Specific surgical approaches are highlighted in each section.