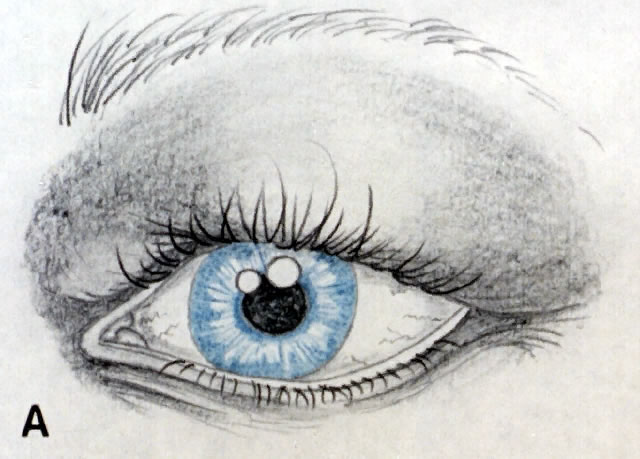
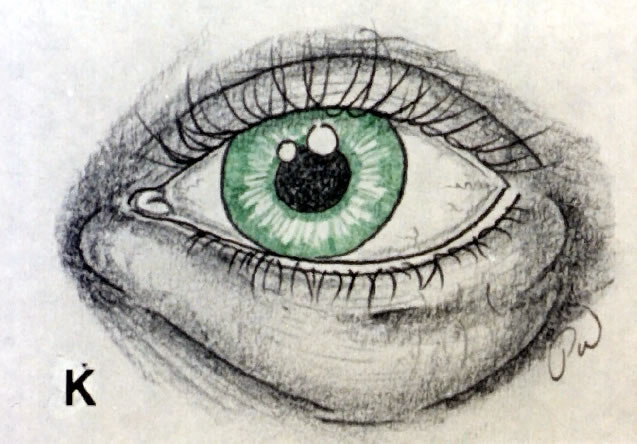
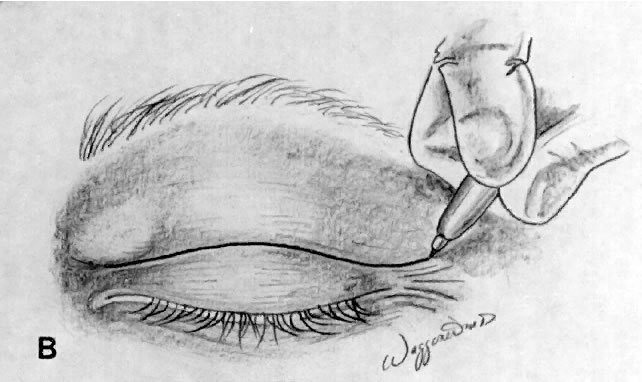
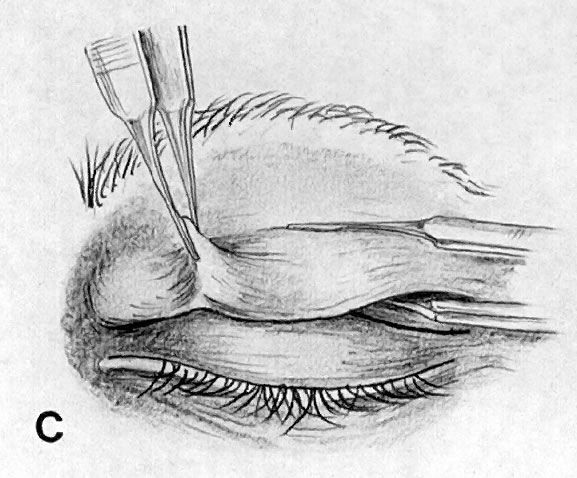
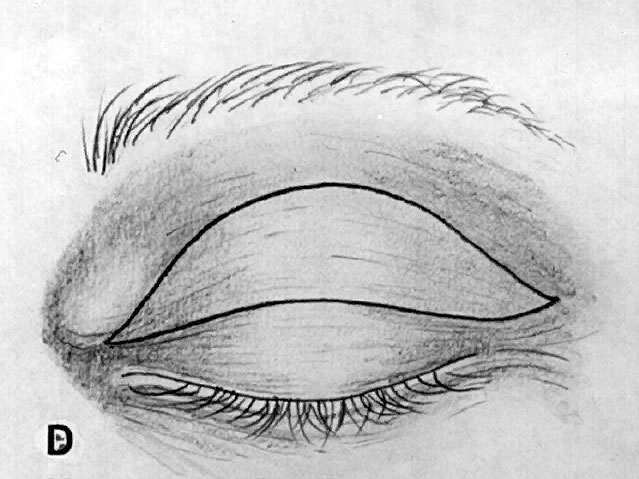
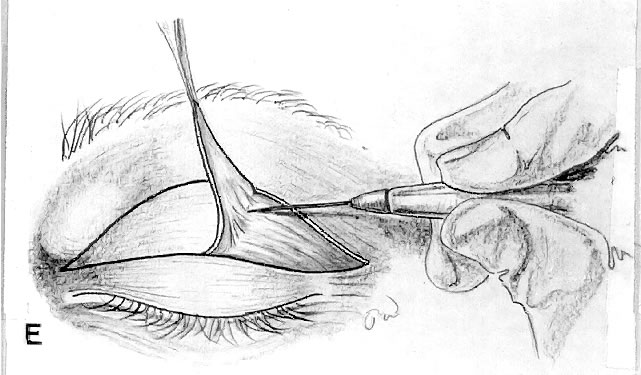
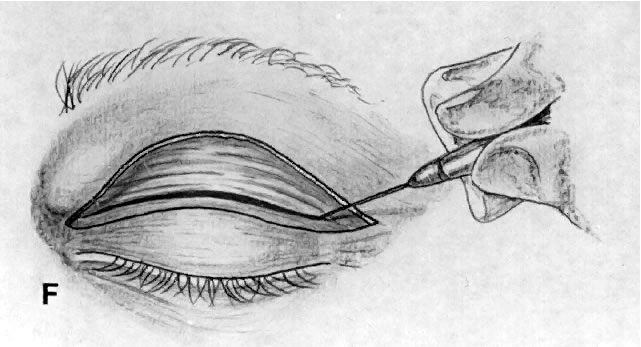
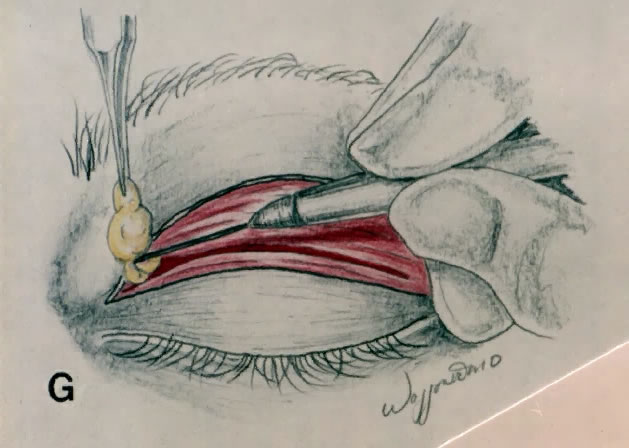
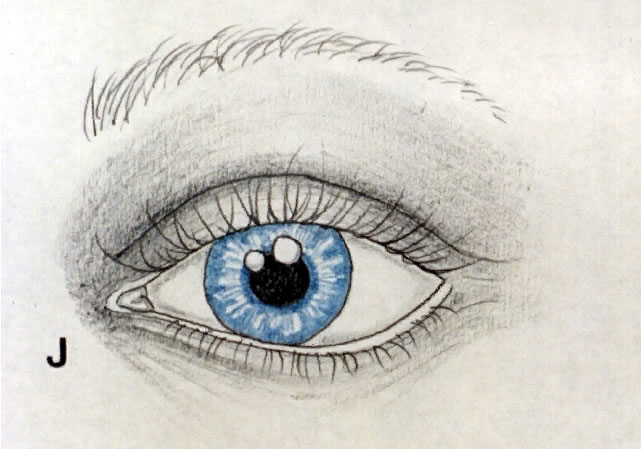
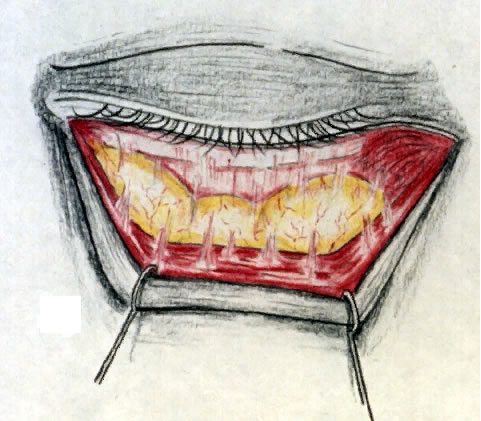
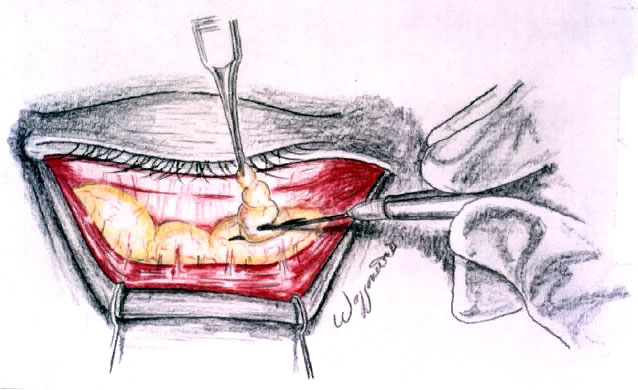
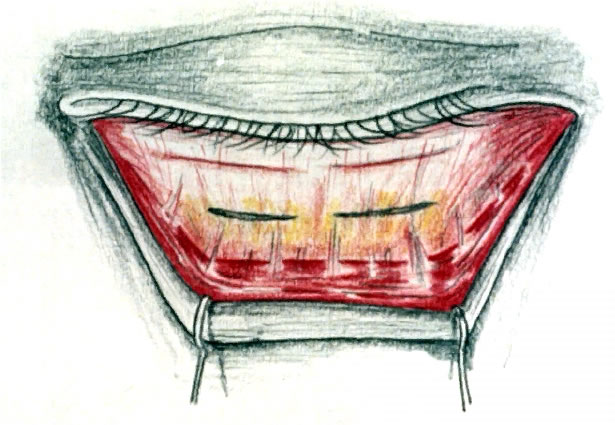
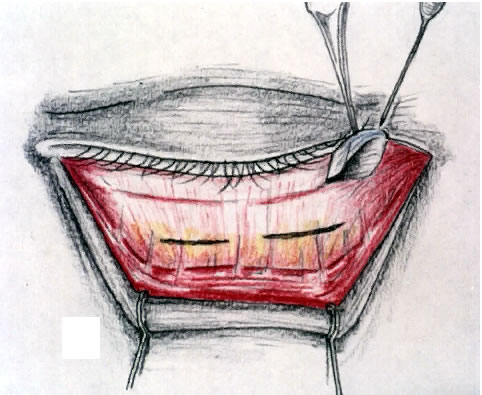
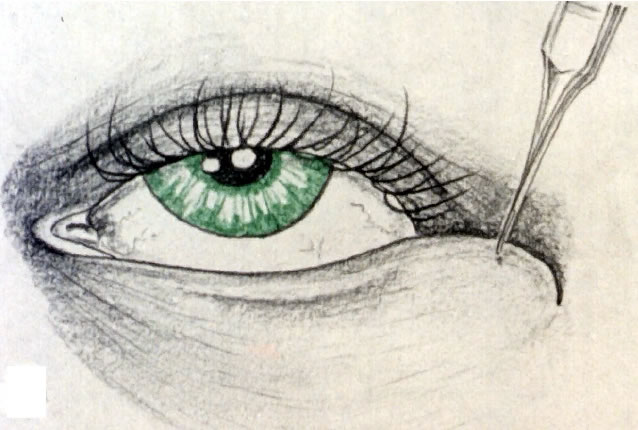
The entire face is examined with subjective quantification of dermatochalasis and steatoblepharon (Fig. 1; see also Fig. 11). Dermatochalasis is baggy eyelid skin, and steatoblepharon is orbital fat that bulges through a thinned orbital septum. There are two primary fat pockets in the upper lid, with the most prominent being the nasal Bourrelet senilis. In the lower lid, the lateral fat pocket is also the smaller and usually less prominent of the two. A coexistent brow ptosis, or blepharoptosis, should be recognized. Additional procedures such as ptosis repair or elevation of the brow may be required at the time of surgery. It may be difficult to convince a patient that a postoperative ptosis was indeed present before surgery unless the patient was evaluated specifically for, and informed preoperatively of, this condition. Likewise, a patient will be disappointed if a functional loss persists after blepharoplasty because a ptotic brow or aponeurotic dehiscence was the true culprit.
|
|
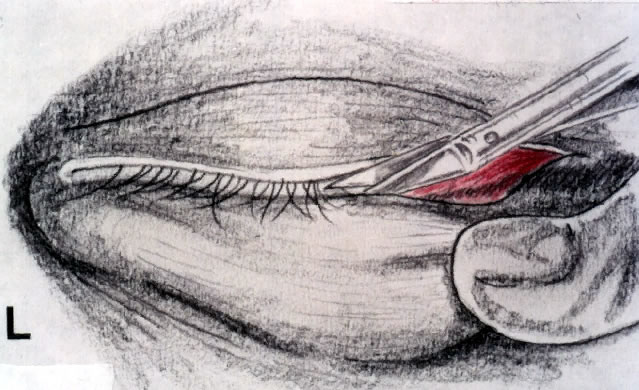
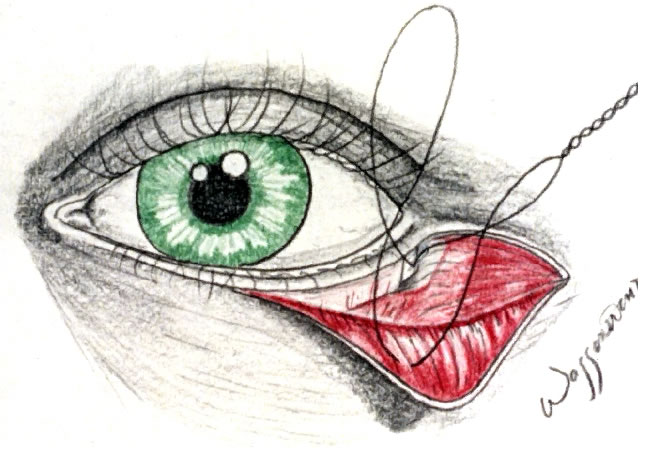
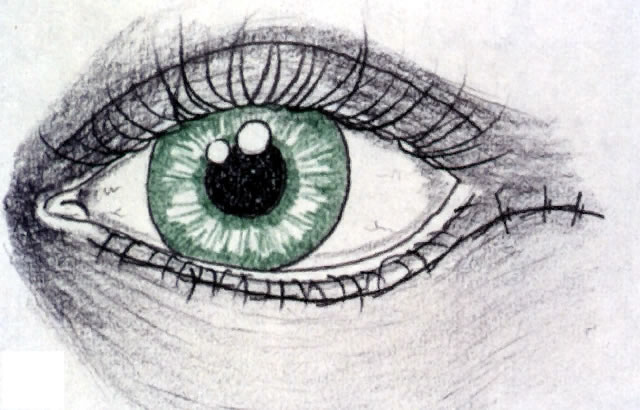
The examination should then focus on specific findings that might increase the risk of complications, such as ectropion, entropion, or exposure keratopathy. One should evaluate for increased horizontal lid laxity or dehiscence of the lower lid retractors.3 The latter is confirmed when the tarsus remains vertical instead of turning out when the lower lid is pulled down and is associated with an abnormal white line in the fornix. If necessary, a horizontal tightening procedure with or without retractor repair may be incorporated at the time of lower lid blepharoplasty. Any history of dry eyes or clinical finding of lagophthalmos, lid retraction, altered blink, or punctate corneal staining may necessitate further evaluation of the tear breakup time and tear output, since additional exposure may be detrimental to an already compromised cornea. Preoperative and postoperative photographs are an integral part of the patient's medical record. They serve as a learning instrument to the surgeon and are paramount in documentation for medicolegal and insurance purposes. By making certain that the patient's brow is relaxed and the excess skin is illustrated, photographs will reinforce findings on clinical examination and visual field testing. Preoperative 35-mm photographs or slides are taken, and they are repeated 1 to 2 months after surgery. A Polaroid photograph taken before surgery is useful during surgery and for immediate use.