|
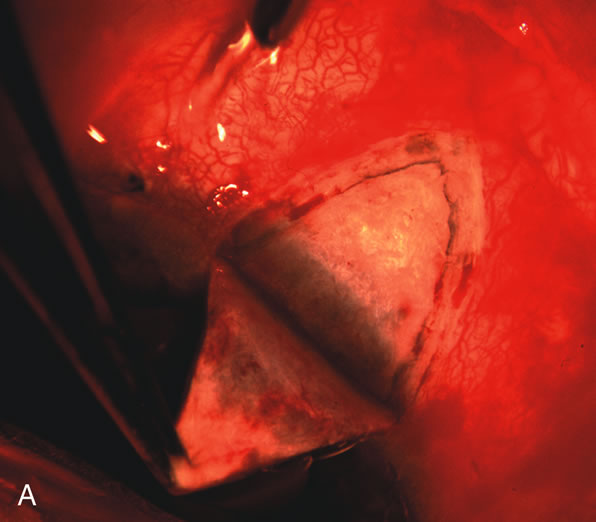
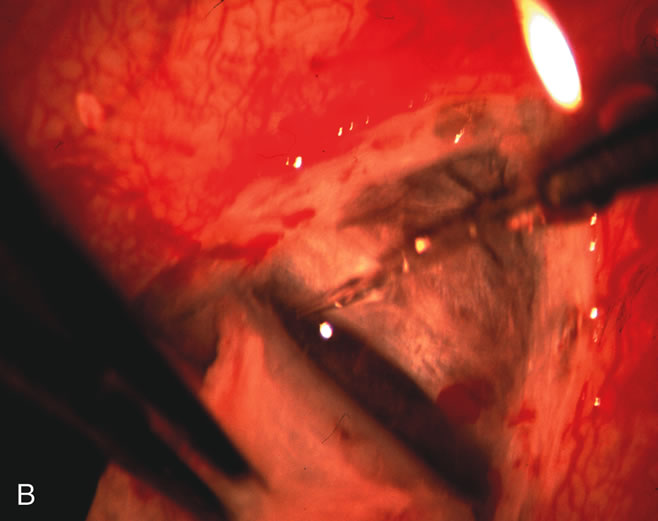
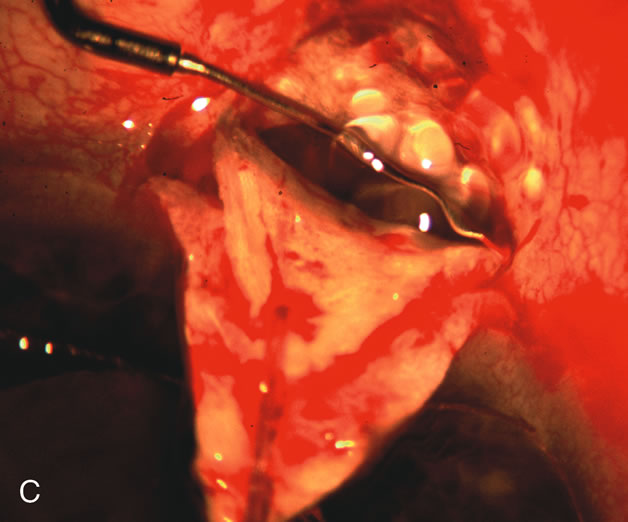
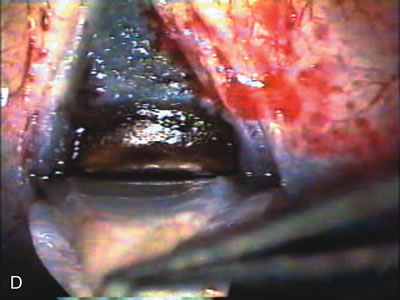
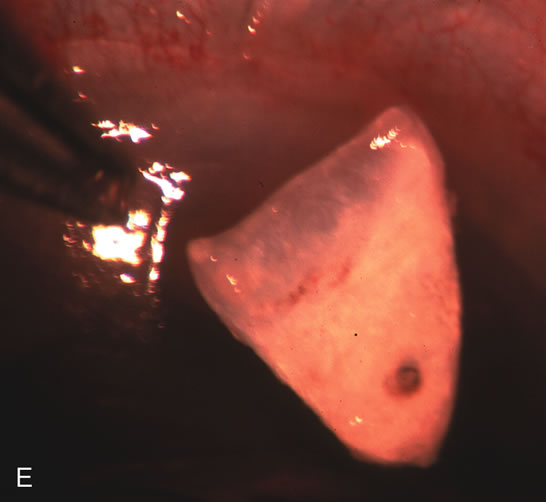
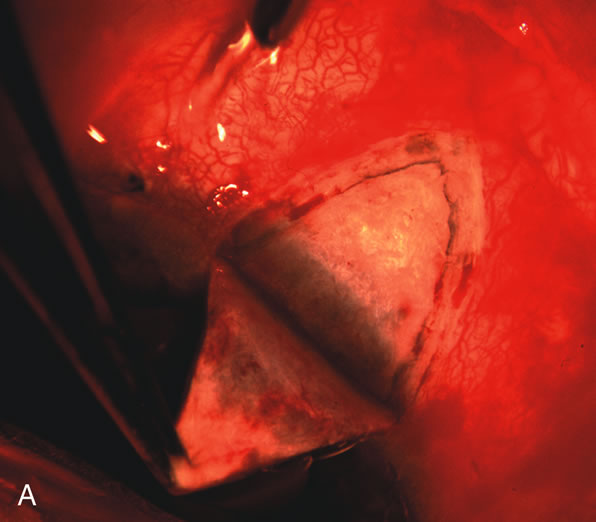
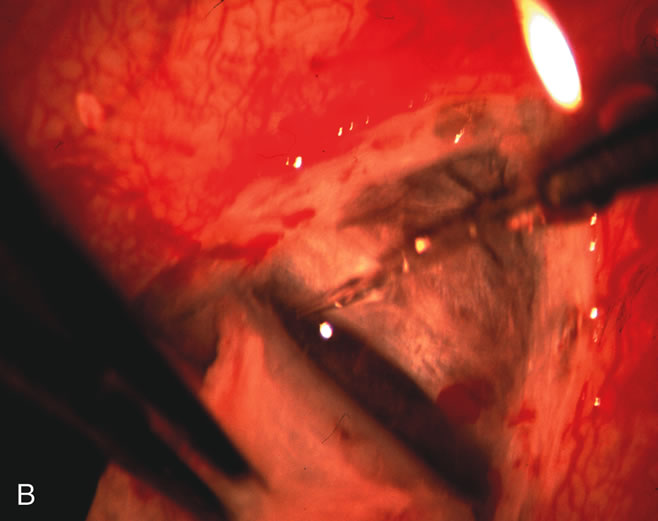
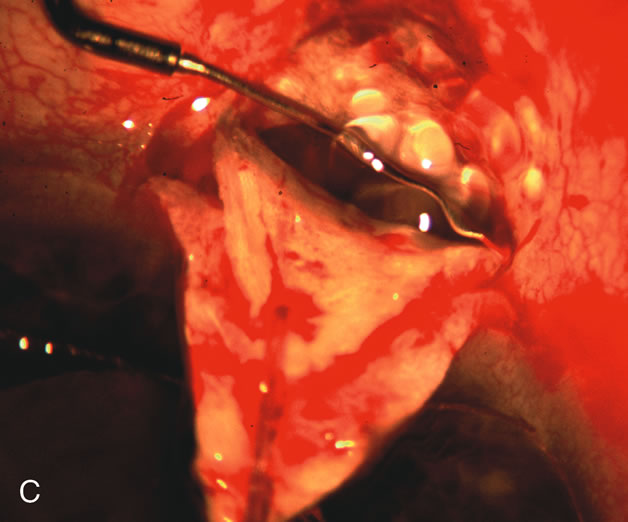
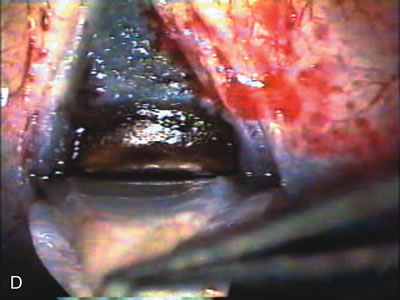
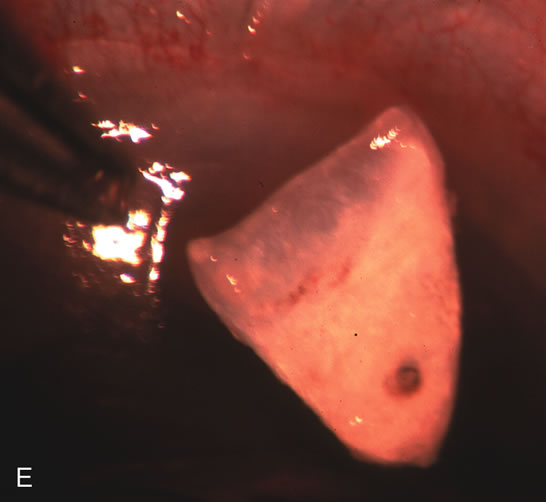
| Fig. 4. Viscocanalostomy with deep sclerectomy and phacoemulsification. Nonpenetrating filtration procedures (NPFS) may be combined with phacoemulsification. Patients with mild disc damage and a history of limited topical drug therapy are the best candidates. Patients who require an IOP in the low teens are not good candidates for NPFS. By definition, NPFS is designed to lower IOP without penetrating into the anterior chamber, thereby avoiding the complications associated with trabeculectomy. Viscocanalostomy is intended to allow aqueous to percolate through a trabeculodescemetic membrane into a subscleral cavern created by the deep sclerectomy. The aqueous diffuses from the cavern into the dilated ostia of Schlemm's canal and into the episcleral venous plexus. A. Fashion a uniform 300-micron superficial scleral flap 1 mm into clear cornea. B. Construct a second 600-micron deep flap that facilitates the unroofing of Schlemm's canal, seen as the darker area. C. Use viscoelastic to dilate the ostia of Schlemm's canal. The major problem with viscocanalostomy is the eventual closure of the ostium decreasing flow to the episcleral plexus. D. Dissect the deep flap anteriorly into clear cornea creating the trabeculodescemetic membrane. This membrane is clearly seen between the scleral spur and the bend of the deep flap. The integrity of this membrane ensures the nonpenetrating portion of the surgery. Another problem with NPFS is the eventual fibrosis of this initially transparent membrane requiring goniopuncture. E. Deep sclerectomy gets its name from removal of the deep flap. Removal of this flap creates the potential subscleral space for accumulation of aqueous before it enters Schlemm's canal and exits the episcleral venous plexus. After removal of the deep flap, the superficial flap is sutured into place and conjunctiva closed. Approximately half of these procedures develop a shallow bleb. |