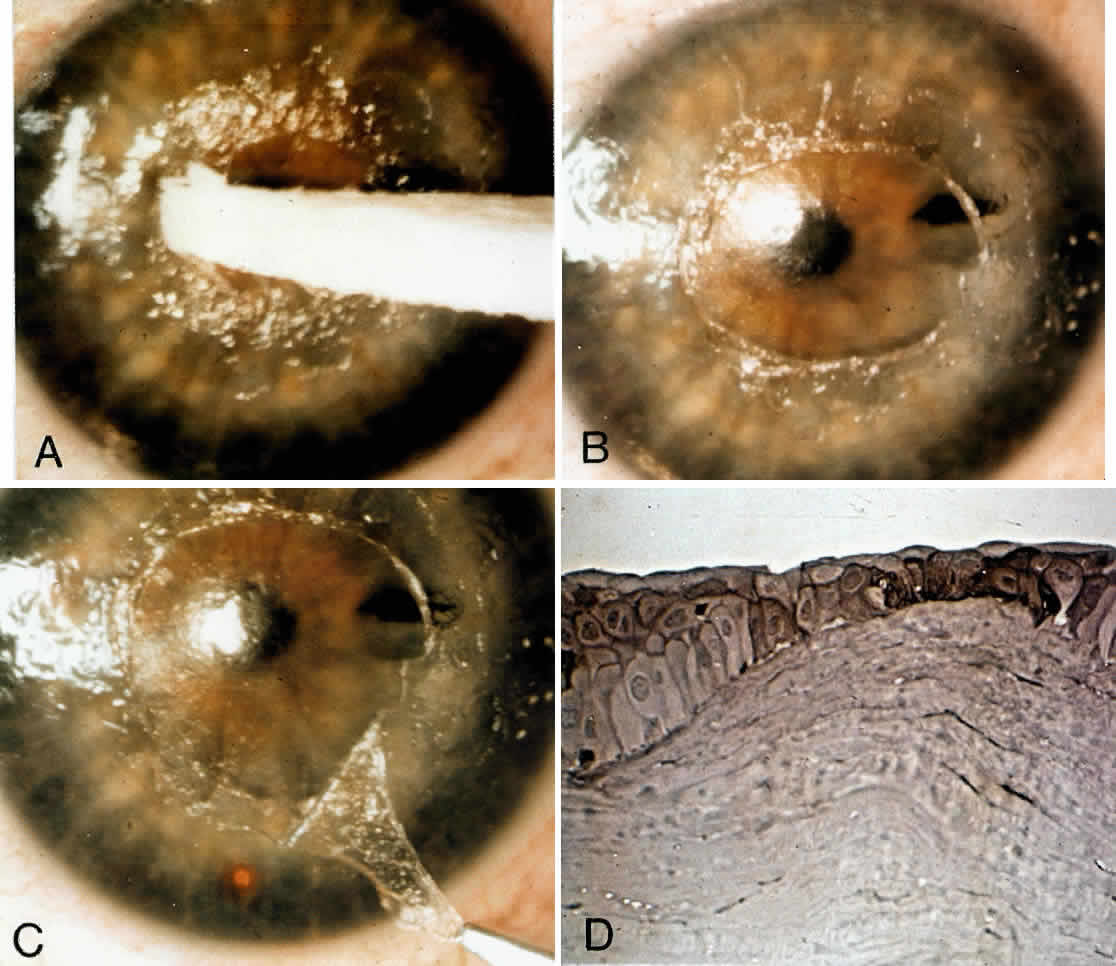
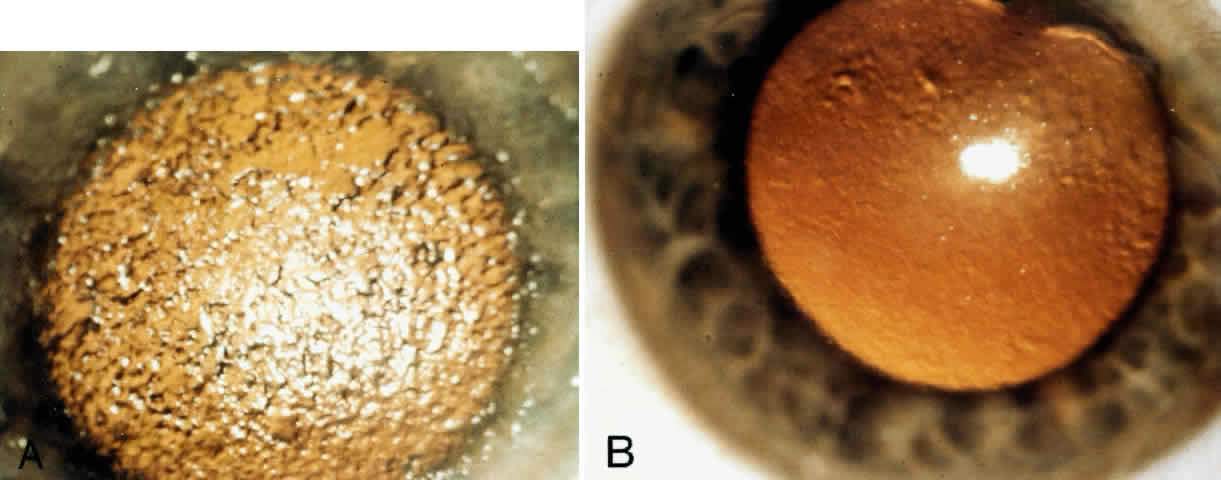
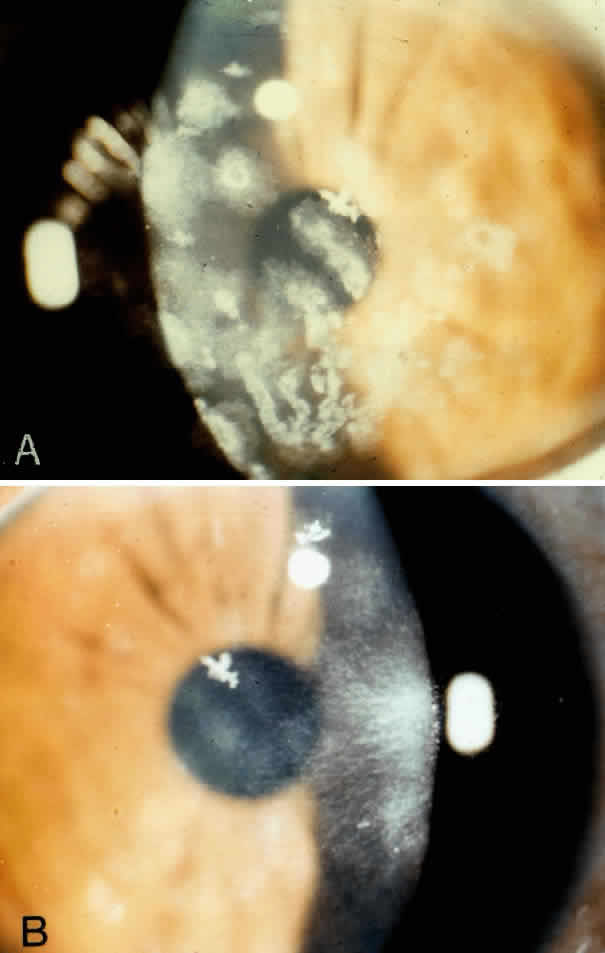
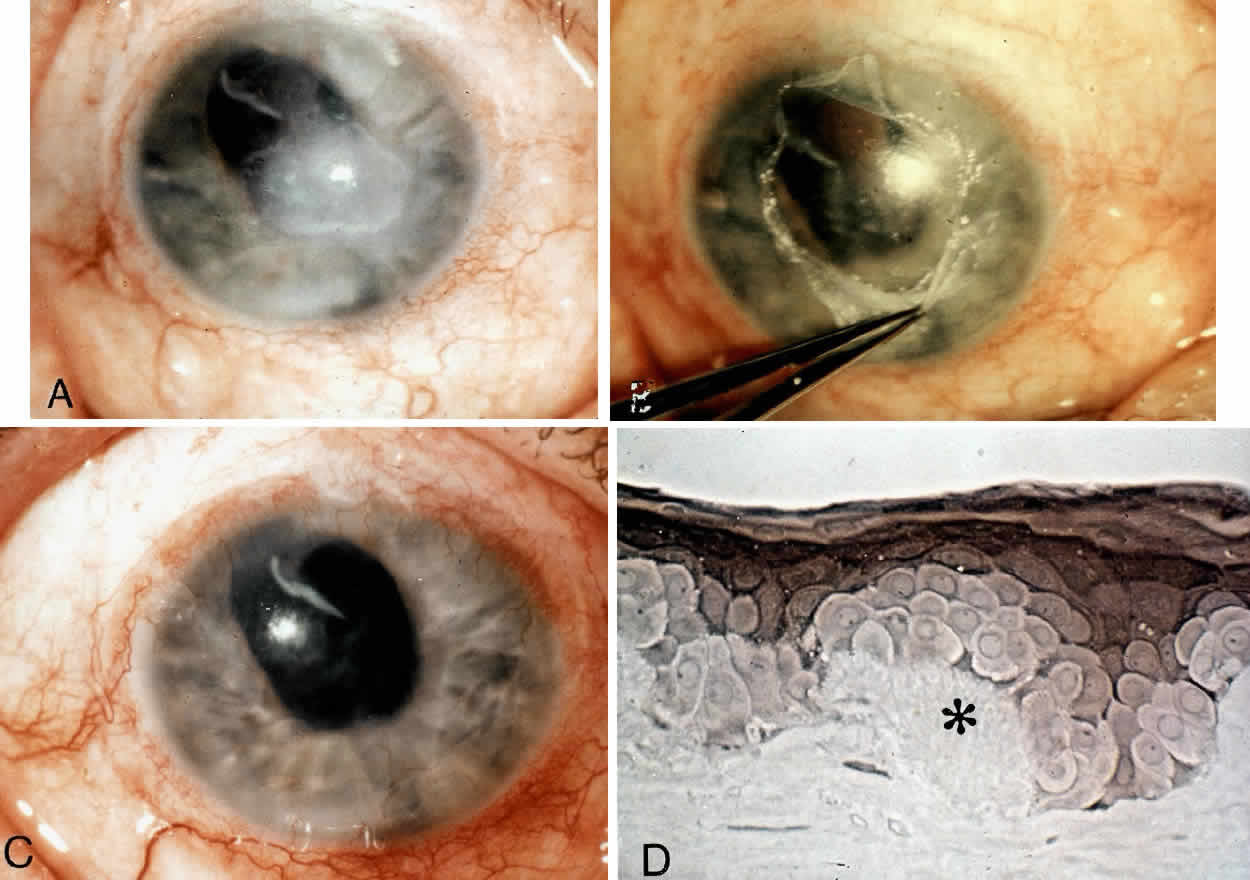
The corneal epithelium is removed over the involved area by gently scraping with a dry cellulose sponge (Weck-cel) or a disposable scarifier blade (Grieshaber 681.01 or Beaver 59). After epithelial removal, the surface should be kept dry to facilitate visualization of subepithelial fibrous plaques or focal accumulations of aberrant basement membrane material. With the aid of a dry cellulose sponge, cleavage planes between the subepithelial fibrous tissue and Bowman's layer can often be located and exploited. After an edge of the subepithelial fibrous membrane is identified, the tissue can be stripped and peeled with the aid of jeweler's forceps, frequently as a continuous sheet, thereby leaving Bowman's layer unharmed. A scarifier may be used to gently scrape or dissect more firmly adherent tissue. Sharp incision or dissection should be avoided to prevent damage to the underlying Bowman's layer or stroma. The cleared corneal surface can be polished with a cellulose sponge or lightly scraped with a scarifier (Fig. 1).1
Postoperatively, antibiotic ointment is applied and the eye is pressure-patched for 24 hours. Thereafter, antibiotic ointment is initially applied four times a day and reduced in frequency over 2 weeks. Re-epithelialization is usually complete in 5 to 7 days. Contact lens wear can be resumed after 2 weeks.