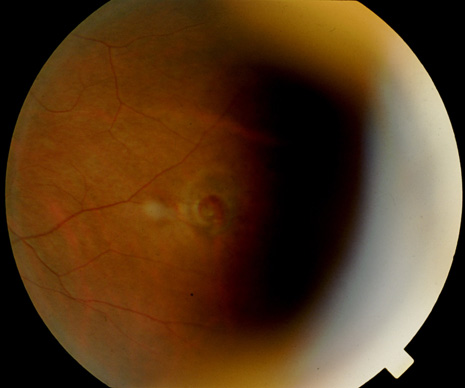
An asymptomatic retinal tear is a full-thickness retinal break not associated with symptoms. Significant evidence suggests that patients with asymptomatic retinal tears may be observed.3–6 In fact the effectiveness of treating asymptomatic retinal tears in preventing RRD is unproved.7,8 Retrospective analyses have shown that subsequent posterior vitreous separation in eyes with preexisting asymptomatic retinal tears does not predispose to subsequent RRD.6 However, the prophylactic treatment of some retinal tears may be considered.
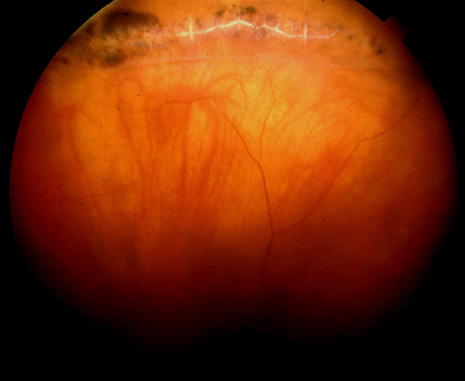
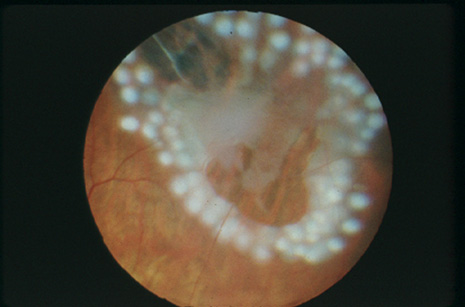
Recent evidence suggests that the fellow eye of patients with RRD is at considerable risk of developing rhegmatogenous events.9 Treatment of fellow eyes of patients with RRD can be considered, but RRD can still arise despite prophylactic laser.10 Patients with RRD caused by giant retinal tears (GRT, tear encompassing greater than 3 clock hours) are a specific subgroup of patients at risk for rhegmatogenous events in the fellow eye. Some recent evidence suggests prophylactic 360-degree cryotherapy treatment in the fellow eye of patients with RRD caused by spontaneous GRT should be considered but this is not universally accepted.11
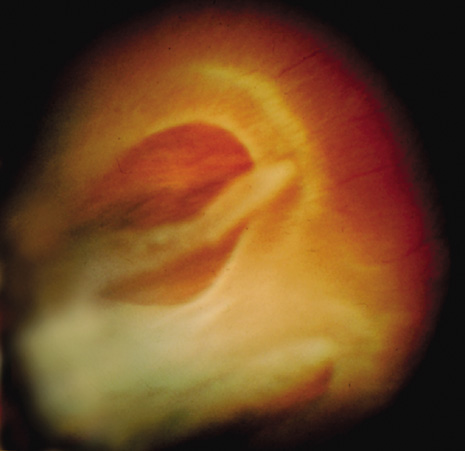
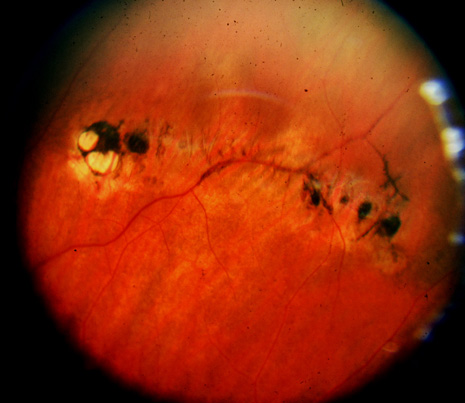
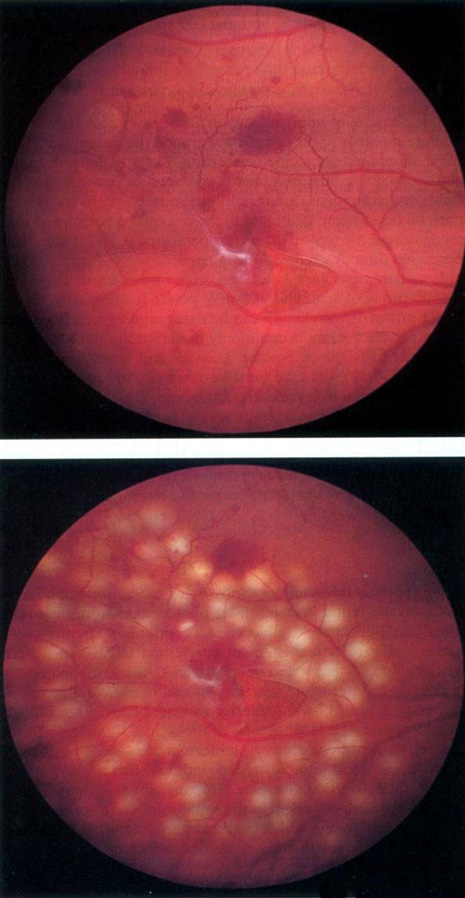
Prophylactic treatment of patients planning on undergoing other ocular procedures can be considered. Asymptomatic retinal tears or extensive lattice (Fig. 3) with traction (Fig. 4) may warrant prophylactic treatment prior to intraocular surgery such as cataract extraction with intraocular lens implant. Prophylactic treatment of myopic eyes prior to LASIK is controversial but may be considered if extensive lattice and/or traction exist. Recent evidence suggests that prophylactic treatment of asymptomatic retinal tears be considered prior to yttrium-aluminum garnet (YAG) laser posterior capsulotomy in high-risk eyes with axial myopia.12