EARLY DEVELOPMENT OF THE EMBRYO
A general understanding of the development of the embryo facilitates an understanding of the development of the eyelids. The fertilized ovum is the original cell, which undergoes several divisions to form a solid clump of cells called a morula. The morula then enlarges and forms a central cavity, to become known as a blastula or blastodermic vesicle (Fig. 1). The outer wall of the blastula forms the placenta. The blastodermic vesicle embeds itself in the uterine mucosa, enlarges, and forms two cavities—each with a single layer of cuboidal epithelium. The upper cavity is the amnion, the lower is the archenteron or yolk sac. The embryo develops from the embryonic plate at the area of contact between the two. At this stage, the embryonic plate consists of two layers: an outer or dorsal ectoderm (epithelial lining of the amnion) and an inner or ventral entoderm (epithelial lining of the yolk sac). A central depression (the primitive streak) followed by a groove develops on the ectodermal surface of the embryonic plate. A middle layer (intraembryonic mesoderm) appears, thus dividing the embryonic plate into three germinal layers from which all tissues of the body develop. The neural groove closes to form the neural canal (24th day). The surface ectoderm within the neural canal is known as the neuroectoderm.1–3
|
At the anterior end of the embryonic plate, three headfolds form: the forebrain, the midbrain, and the hindbrain. At the front of the forebrain, a small depression is noted on each side of the midline. This depression is the anlage of the eye and is called the optic pit. Toward the end of the third week of gestation, the optic pit deepens until it contacts the surface ectoderm and becomes the primary optic vesicle. At this stage, the eyes are at the side of the head at an angle of 180° (Fig. 2). The embryo consists of a head with the three divisions of the brain, a segmented body with spinal canal, and a tailfold. That portion of the mesoderm closest to the spinal canal is known as paraxial mesoderm. The primary optic vesicle then undergoes invagination to form the secondary optic vesicle or the optic cup. This starts at 2.5 weeks' gestation and is complete by 1 month.3–5
|
SEGMENTATION
Humans are segmented beings. Segmentation begins simultaneously with closure of the neural groove (24th day). Segmentation extends posteriorly and anteriorly to the head region, where segmentation is lost. Instead, five branchial or pharyngeal arches form. At 5 weeks' gestation, a sheet of immature mesoderm originates from the first branchial arch (“mandibular arch”). The first branchial arch consists of a small dorsal portion known as the maxillary process, which extends forward beneath the eye to develop into the lower eyelid. Cephalad to the first branchial arch, mesenchymal proliferation creates other folds that form other facial processes: the frontonasal, medial nasal, lateral nasal, and mandibular processes (Fig. 3).1–8
EYELID FORMATION
The maxillary process lies in apposition to the paraxial mesoderm of the eye and the nasal process. Between them is a groove of thickened ectoderm, which becomes buried as the maxillary process overgrows the nasal process. This occurs at 5 weeks' gestation and is the first indication of the nasolacrimal duct. The maxillary process extends superiorly to form the lower eyelid at 6 weeks' gestation. In doing so, the inner end folds in a layer of ectodermal tissue that is continuous with the nasolacrimal duct at its lower end. Before the lower lids are apparent, the upper lids are formed by an extension of orbital or paraxial mesoderm known as the frontonasal process. Thus, the upper lid arises from the frontonasal process slightly before the lower lid arises from the maxillary process. The inner end of the upper lid also folds in a portion of ectodermal plate, which forms the upper canaliculus. This unites with the lower canaliculus at the upper end of the nasolacrimal duct.6–8
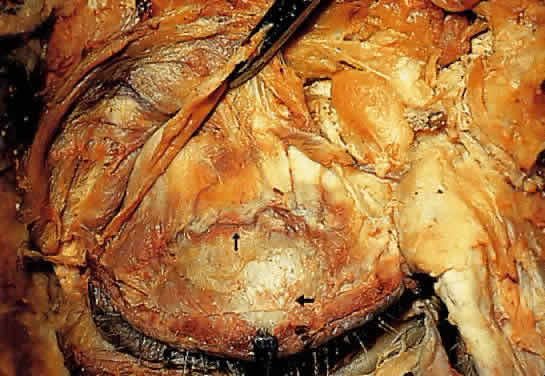
LID FUSION
At 1.5 months' gestation, the lateral canthus is formed by the union of the upper and lower eyelid folds. The two lids come together and temporarily fuse from within outward at 8 weeks' gestation (Fig. 4A). Closure is complete at 10 weeks' gestation. Desmosomal adhesions between the lid margins isolate the eye from the amniotic fluid.1 All lid structures are formed during this period of adhesion (Fig. 4B). Riolan's muscle can be identified by the end of the third month. Hair bulbs of eyelashes appear first in the upper lids, then in the lower lids in an anteroposterior direction.2 Development is slightly more advanced in the upper lid, compared with the lower. At the beginning of the fourth month, the meibomian glands begin to appear. The posterior half of the lid shows a greater condensation of basal lamina and collagen fibers, indicating the tarsal plate region. The meibomian glands grow into the tarsal plates—first in the upper then in the lower lids. The apocrine Moll's glands also appear around the cilia follicles during the fourth month, followed shortly by the sebaceous glands of Zeis.3,6
|
At 2.5 months' gestation, the levator palpebrae superioris develops. It separates from the superior rectus muscle at the fourth month of gestation. Clinically, failure of separation of these muscles would result in congenital ptosis.
LID DYSJUNCTION
At the end of the fifth month (weeks 21 to 26 gestation), the epithelial adhesions between the lids begin to break down (see Fig. 4C). This process is usually completed by the sixth month but may persist until shortly before birth. Holocrine production of lipids from the meibomian glands, keratinization of the lid margin, and pull of the developing eyelid retractors are responsible for the dysjunction.7,8
ABNORMALITIES OF EYELID DEVELOPMENT
When normal progression of lid development is interrupted, a spectrum of congenital anomalies occurs.8,9
Cryptophthalmia (ablepharon)—absence of the eyelid—is due to failure of the eyelid folds to embryologically develop. The cornea undergoes metaplasia and is covered with skin, which passes continuously from the forehead to the cheek. Most are sporadic but a recessive inheritance pattern has been suggested.10 Cryptophthalmia occurs bilaterally twice as often as unilaterally and is slightly more common in males. It can be associated with ear and nose malformations, cleft lip and palate, hypertelorism, laryngeal atresia, lacrimal duct defects, renal anomalies, syndactyly, and meningoencephalocele.11
Microblepharia is an incomplete lid development wherein the eyeball is not covered, resulting in congenital lagophthalmos.
Coloboma of the eyelid is a defect in the lid margin, with absence of lashes and glands. The most common site is in the upper lid at the junction of the inner third and the outer two thirds. In the lower eyelid, it is more frequently seen at the junction of the outer third and the inner two thirds. These abnormalities may be due to the formation and pressure of amniotic bands or from failure of the eyelids to fuse during embryonic life. This may be associated with cleft palate, mandibulofacial dysotosis, limbal dermoids, lipodermoids, iris colobomas, or brow colobomas.9
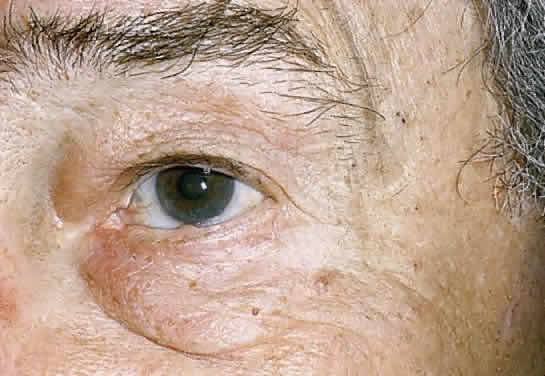
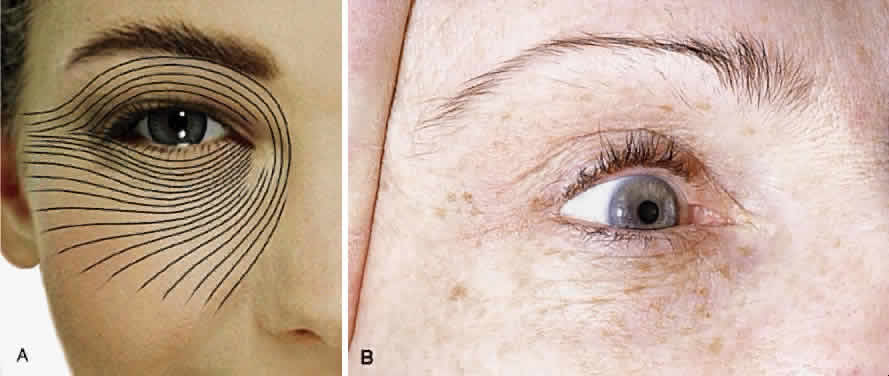
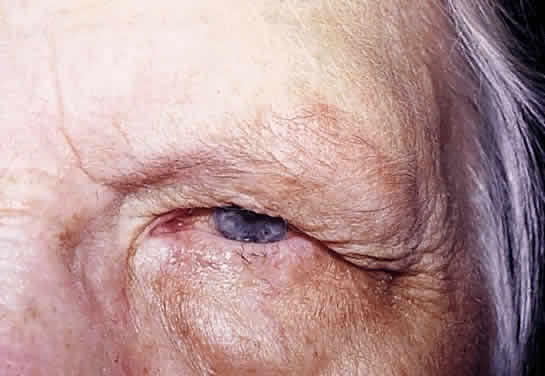
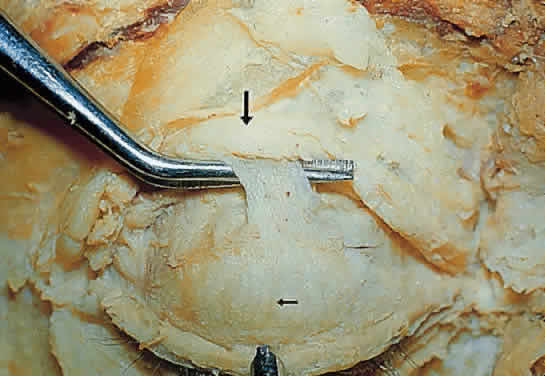
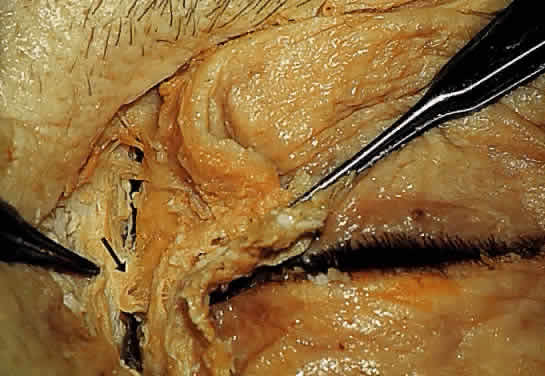
Epicanthus is a fold of skin that extends from the side of the nose to the upper lid and partially hides the inner canthus. This condition is normally present in the embryo and early infancy. Frequently, it is associated with ptosis, although it may occur independently. Epicanthus is usually bilateral but may be asymmetric or unilateral. There are four known types, depending on the origin of the upper end of the fold. In epicanthus superciliaris, the fold arises in the region of the eyebrow and extends over the lacrimal sac. Epicanthus palpebralis (Fig. 5) has an epicanthal fold arising from the upper tarsal area, extending toward the lower margin of the orbit. The fold is equally distributed in the upper and lower lids. In epicanthus tarsalis (Fig. 6), the epicanthal fold arises from the tarsal fold and ends close to the inner canthus. Thus, the fold is more prominent in the upper lid. It is a normal variation of the Asian eyelid. In epicanthus inversus, (Fig. 7) the fold arises in the lower lid and extends upward, partially covering the inner canthus, usually terminating in the upper lid.
|
|
|
Congenital ptosis is most commonly seen because of the absence or fibrotic nature of the levator palpebrae superioris. It may be unilateral or bilateral and associated with weakness of the superior rectus muscle from which the levator is derived. In the “jaw winking” phenomena, ptosis appears when the patient chews. This is due to an abnormal association of the nerve to the levator muscle and the nerve to the external pterygoid muscle.
Many abnormalities exist of eyelid margin differentiation. Distichiasis is a condition in which aberrant lashes develop at or near the orifices of the meibomian glands. Ankyloblepharon is an abnormal fusion of the lid margins from incomplete separation of the lid folds. The fusion may be complete but is more common at the inner canthus. A variant is “ankyloblepharon filiform adnatum,” in which the lid margins are connected by multiple fine bands. Blepharophimosis is a horizontal narrowing of the palpebral aperture. The triad of blepharophimosis syndrome includes ptosis, horizontal shortening of the palpebral fissures, and epicanthus inversus (Fig. 7). Telecanthus, lower eyelid entropion or ectropion, hypoplasia of the superior orbital rims, a poorly developed nasal bridge, and hypertelorism can also be seen with this condition.
Epiblepharon is an additional fold of skin running horizontally below the lower eyelid margin. It often is associated with loss of the eyelid crease and may be partly due to a lack of deep anchoring of the superficial skin to the orbicularis oculi muscle. The weight of the skin fold may rotate the lower lid margin inward, creating an entropion. With growth of the face and nasal bridge, epiblepharon usually diminishes. It is seen more commonly in Asian eyelids.
Euryblepharon is a rounding or almond-shaped deformity of the lower lid at the lateral canthal angle. It may be associated with an inferiorly displaced lateral canthal tendon.
Congenital entropion is characterized by an inward turning of the eyelid margin due to hypertrophy of the orbicularis muscle, defects in lower lid retractor, or tarsal abnormalities.12
Congenital ectropion is characterized by eversion of the eyelid margin. It is rarely seen in the upper lid. In the lower lid, it is usually seen with Down's syndrome or blepharophimosis syndrome.