|
|
Chapter 5: Conjunctiva
Authors:
Conjunctiva
I. CONJUNCTIVITIS
Inflammation of the conjunctiva (conjunctivitis) is the most common eye disease worldwide. It varies in severity from a mild hyperemia with tearing to a severe conjunctivitis with copious purulent discharge. The cause is usually exogenous, but rarely it may be endogenous.
CONJUNCTIVITIS DUE TO INFECTIOUS AGENTS
The types of conjunctivitis and their commonest causes are set forth in Tables 5-1 and 5-2.
Because of its location, the conjunctiva is exposed to many microorganisms and other stressful environmental factors. Several mechanisms protect the surface of the eye from external substances: In the tear film, the aqueous component dilutes infectious material, mucus traps debris, and a pumping action of the lids constantly flushes the tears to the tear duct; the tears contain antimicrobial substances, including lysozyme and antibodies (IgG and IgA).
Common pathogens that can cause conjunctivitis include Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Neisseria meningitidis, most human adenovirus strains, herpes simplex virus type 1 and type 2, and two picornaviruses. Two sexually transmitted agents that cause conjunctivitis are Chlamydia trachomatis and Neisseria gonorrhoeae.
Cytology of Conjunctivitis
Damage to the conjunctival epithelium by a noxious agent may be followed by epithelial edema, cellular death and exfoliation, epithelial hypertrophy, or granuloma formation. There may also be edema of the conjunctival stroma (chemosis) and hypertrophy of the lymphoid layer of the stroma (follicle formation). Inflammatory cells, including neutrophils, eosinophils, basophils, lymphocytes, and plasma cells, may be seen and often indicate the nature of the damaging agent. The inflammatory cells migrate from the conjunctival stroma through the epithelium to the surface. They then combine with fibrin and mucus from the goblet cells to form the conjunctival exudate, which is responsible for the "mattering" on the lid margins (especially in the morning).
The inflammatory cells appear in the exudate or in scrapings taken with a sterile platinum spatula from the anesthetized conjunctival surface. The material is stained with Gram's stain (to identify the bacterial organisms) and with Giemsa's stain (to identify the cell types and morphology). A predominance of polymorphonuclear leukocytes is characteristic of bacterial conjunctivitis. Generally, a predominance of mononuclear cells-especially lymphocytes-is characteristic of viral conjunctivitis. If a pseudomembrane or true membrane is present (eg, epidemic keratoconjunctivitis or herpes simplex virus conjunctivitis), neutrophils then predominate because of coexistent necrosis. In chlamydial conjunctivitis, neutrophils and lymphocytes are usually present in equal numbers.
In allergic conjunctivitis, eosinophils and basophils are frequently present in conjunctival biopsies, but they are less common on conjunctival smears; eosinophils or eosinophilic granules are commonly found in vernal keratoconjunctivitis. High levels of proteins secreted by eosinophils (eg, eosinophil cationic protein) can be found in the tears of patients with vernal, atopic, or allergic conjunctivitis. Eosinophils and basophils are found in allergic conjunctivitis, and scattered eosinophilic granules and eosinophils are found in vernal keratoconjunctivitis. In all types of conjunctivitis, there are plasma cells in the conjunctival stroma. They do not migrate through the epithelium, however, and are therefore not seen in smears of exudate or of scrapings from the conjunctival surface unless the epithelium has become necrotic, as it may in trachoma; in this event, the rupturing of a follicle allows the plasma cells to reach the epithelial surface. Since the mature follicles of trachoma rupture easily, the finding of large, pale-staining lymphoblastic (germinal center) cells in scrapings strongly suggests trachoma.
Symptoms of Conjunctivitis
The important symptoms of conjunctivitis are a foreign body sensation, a scratching or burning sensation, a sensation of fullness around the eyes, itching, and photophobia.
Foreign body sensation and a scratching or burning sensation are often associated with the swelling and papillary hypertrophy that normally accompany conjunctival hyperemia. If there is pain, the cornea is probably also affected. Pain of the iris or ciliary body is also suggestive of corneal involvement.
Signs of Conjunctivitis (Table 5-2)
The important signs of conjunctivitis are hyperemia, tearing, exudation, pseudoptosis, papillary hypertrophy, chemosis, follicles, pseudomembranes and membranes, granulomas, and preauricular adenopathy.
Hyperemia is the most conspicuous clinical sign of acute conjunctivitis. The redness is most marked in the fornix and diminishes toward the limbus by virtue of the dilation of the posterior conjunctival vessels. (A perilimbal dilation or ciliary flush suggests inflammation of the cornea or deeper structures.) A brilliant red suggests bacterial conjunctivitis, and a milky appearance suggests allergic conjunctivitis. Hyperemia without cellular infiltration suggests irritation from physical causes such as wind, sun, smoke, etc, but may occur occasionally with diseases associated with vascular instability (eg, acne rosacea).
Tearing (epiphora) is often prominent in conjunctivitis, the tears resulting from the foreign body sensation, the burning or scratching sensation, or the itching. Mild transudation also arises from the hyperemic vessels and adds to the tearing. An abnormally scant secretion of tears and an increase in mucous threads suggests keratoconjunctivitis sicca.
Exudation is a feature of all types of acute conjunctivitis. The exudate is flaky and amorphous in bacterial conjunctivitis and stringy in allergic conjunctivitis. "Mattering" of the eyelids occurs upon awakening in almost all types of conjunctivitis, and if the exudate is copious and the lids are firmly stuck together, the conjunctivitis is probably bacterial or chlamydial.
Pseudoptosis is a drooping of the upper lid secondary to infiltration of Müller's muscle. The condition is seen in several types of severe conjunctivitis, eg, trachoma and epidemic keratoconjunctivitis.
Papillary hypertrophy is a nonspecific conjunctival reaction that occurs because the conjunctiva is bound down to the underlying tarsus or limbus by fine fibrils. When the tuft of vessels that forms the substance of the papilla (along with cellular elements and exudates) reaches the basement membrane of the epithelium, it branches over the papilla like the spokes in the frame of an umbrella. An inflammatory exudate accumulates between the fibrils, heaping the conjunctiva into mounds. In necrotizing disease (eg, trachoma), the exudate may be replaced by granulation tissue or connective tissue.
When the papillae are small, the conjunctiva usually has a smooth, velvety appearance. A red papillary conjunctiva suggests bacterial or chlamydial disease (eg, a velvety red tarsal conjunctiva is characteristic of acute trachoma). With marked infiltration of the conjunctiva, giant papillae form which are flat-topped, polygonal, and milky-red in color. On the upper tarsus, they suggest vernal keratoconjunctivitis and giant papillary conjunctivitis with contact lens sensitivities; on the lower tarsus, they suggest atopic keratoconjunctivitis. Giant papillae may also occur at the limbus, especially in the area that is normally exposed when the eyes are open (between 2 and 4 o'clock and between 8 and 10 o'clock). Here they appear as gelatinous mounds that may encroach on the cornea. Limbal papillae are characteristic of vernal keratoconjunctivitis but are rare in atopic keratoconjunctivitis.
Chemosis of the conjunctiva strongly suggests acute allergic conjunctivitis but may also occur in acute gonococcal or meningococcal conjunctivitis and especially in adenoviral conjunctivitis. Chemosis of the bulbar conjunctiva is seen in patients with trichinosis. Occasionally, chemosis may appear before there is any gross cellular infiltration or exudation.
Follicles are seen in most cases of viral conjunctivitis, in all cases of chlamydial conjunctivitis except neonatal inclusion conjunctivitis, in some cases of parasitic conjunctivitis, and in some cases of toxic conjunctivitis induced by topical medications such as idoxuridine, dipivefrin, and miotics. Follicles in the inferior fornix and at the tarsal margins have limited diagnostic value, but when they are located on the tarsi (especially the upper tarsus), chlamydial, viral, or toxic conjunctivitis (following topical medication) should be suspected.
The follicle consists of a focal lymphoid hyperplasia within the lymphoid layer of the conjunctiva and usually contains a germinal center. Clinically, it can be recognized as a rounded, avascular white or gray structure. On slitlamp examination, small vessels can be seen arising at the border of the follicle and encircling it.
Pseudomembranes and membranes are the result of an exudative process and differ only in degree. A pseudomembrane is a coagulum on the surface of the epithelium, and when it is removed the epithelium remains intact. A membrane is a coagulum involving the entire epithelium, and if it is removed a raw, bleeding surface remains. Pseudomembranes or membranes may accompany epidemic keratoconjunctivitis, primary herpes simplex virus conjunctivitis, streptococcal conjunctivitis, diphtheria, cicatricial pemphigoid, and erythema multiforme major. They may also be an aftermath of chemical burns, especially alkali burns.
Ligneous conjunctivitis is a peculiar form of recurring membranous conjunctivitis. It is bilateral, seen mainly in children, predominantly in females, and may be associated with other systemic findings, including nasopharyngitis and vulvovaginitis.
Granulomas of the conjunctiva always affect the stroma and most commonly are chalazia. Other endogenous causes include sarcoid, syphilis, cat-scratch disease, and, rarely, coccidioidomycosis. Parinaud's oculoglandular syndrome includes conjunctival granulomas and a prominent preauricular lymph node, and this group of diseases may require biopsy examination to secure diagnosis.
Phlyctenules represent a delayed hypersensitivity reaction to microbial antigen, eg, staphylococcal or mycobacterial antigens. Phlyctenules of the conjunctiva initially consist of a perivasculitis with lymphocytic cuffing of a vessel. When they progress to ulceration of the conjunctiva, the ulcer bed has many polymorphonuclear leukocytes.
Preauricular lymphadenopathy is an important sign of conjunctivitis. A grossly visible preauricular node is seen in Parinaud's oculoglandular syndrome and, rarely, in epidemic keratoconjunctivitis. A large or small preauricular node, sometimes slightly tender, occurs in primary herpes simplex conjunctivitis, epidemic keratoconjunctivitis, inclusion conjunctivitis, and trachoma. Small but nontender preauricular lymph nodes occur in pharyngoconjunctival fever and acute hemorrhagic conjunctivitis. Occasionally, preauricular lymphadenopathy may be observed in children with infections of the meibomian glands.
BACTERIAL CONJUNCTIVITIS
Two forms of bacterial conjunctivitis are recognized: acute (and subacute) and chronic. Acute bacterial conjunctivitis may be self-limited when caused by certain microorganisms such as Haemophilus influenzae. The course may take up to 2 weeks if proper treatment is not given.
Acute bacterial conjunctivitis may become chronic. Treatment with one of the many available antibacterial agents usually cures the condition in a few days.
Purulent conjunctivitis caused by Neisseria gonorrhoeae or Neisseria meningitidis may lead to serious ocular complications if not treated early.
Clinical Findings
A. Symptoms and Signs:
The organisms listed in Table 5-1 account for most cases of bacterial conjunctivitis. They produce bilateral irritation and injection, a purulent exudate with sticky lids on waking, and occasionally lid edema. The infection usually starts in one eye and is spread to the other by the hands. It may be spread from one person to another by fomites.
1. Hyperacute (and subacute) bacterial conjunctivitis-Purulent conjunctivitis-
(caused by N gonorrhoeae, Neisseria kochii, and N meningitidis) is marked by a profuse purulent exudate (Figure 5-1). Meningococcal conjunctivitis may occasionally be seen in children. Any severe, profusely exudative conjunctivitis demands immediate laboratory investigation and immediate treatment. If there is any delay, there may be severe corneal damage or loss of the eye, or the conjunctiva could become the portal of entry for either N gonorrhoeae or N meningitidis, leading to septicemia or meningitis.
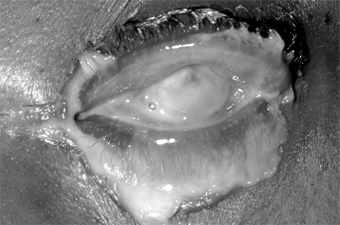
Figure 5-1: Gonococcal conjunctivitis. Profuse purulent exudate. (Courtesy of L Schwab.)
Acute mucopurulent (catarrhal) conjunctivitis often occurs in epidemic form and is called "pinkeye" by most laymen. It is characterized by an acute onset of conjunctival hyperemia and a moderate amount of mucopurulent discharge. The commonest causes are Streptococcus pneumoniae in temperate climates and Haemophilus aegyptius in warm climates. Less common causes are staphylococci and other streptococci. The conjunctivitis caused by S pneumoniae and H aegyptius may be accompanied by subconjunctival hemorrhages. H aegyptius conjunctivitis in Brazil has been followed by a fatal purpuric fever produced by a plasmid-associated toxin of the bacteria.
Subacute conjunctivitis is caused most often by H influenzae and occasionally by Escherichia coli and Proteus species. H influenzae infection is characterized by a thin, watery, or flocculent exudate.
2. Chronic bacterial conjunctivitis-Chronic bacterial conjunctivitis-
occurs in patients with nasolacrimal duct obstruction and chronic dacryocystitis, which are usually unilateral. It may also be associated with chronic bacterial blepharitis or meibomian gland dysfunction. Patients with floppy lid syndrome or ectropion may develop secondary bacterial conjunctivitis.
Rare bacterial conjunctivitides may be caused by Corynebacterium diphtheriae and Streptococcus pyogenes. Pseudomembranes or membranes caused by these organisms may form on the palpebral conjunctiva. The rare cases of chronic conjunctivitis produced by Moraxella catarrhalis, the coliform bacilli, Proteus, etc, are as a rule indistinguishable clinically.
B. Laboratory Findings:
In most cases of bacterial conjunctivitis, the organisms can be identified by the microscopic examination of conjunctival scrapings stained with Gram's stain or Giemsa's stain; this reveals numerous polymorphonuclear neutrophils. Conjunctival scrapings for microscopic examination and culture are recommended for all cases and are mandatory if the disease is purulent, membranous, or pseudomembranous. Antibiotic sensitivity studies are also desirable, but empirical antibiotic therapy should be started. When the results of antibiotic sensitivity tests become available, specific antibiotic therapy can then be instituted.
Complications & Sequelae
Chronic marginal blepharitis often accompanies staphylococcal conjunctivitis except in very young patients who are not subject to blepharitis. Conjunctival scarring may follow both pseudomembranous and membranous conjunctivitis, and in rare cases corneal ulceration and perforation supervene.
Marginal corneal ulceration may follow infection with N gonorrhoeae, N kochii, N meningitidis, H aegyptius, S aureus, and M catarrhalis; if the toxic products of N gonorrhoeae diffuse through the cornea into the anterior chamber, they may cause toxic iritis.
Treatment
Specific therapy of bacterial conjunctivitis depends on identification of the microbiologic agent. While waiting for laboratory reports, the physician can start topical therapy with an antimicrobial drug. In any purulent conjunctivitis in which Gram's stain shows gram-negative diplococci suggestive of Neisseria, both system and topical therapy should be started immediately. If there is no corneal involvement, a single intramuscular dose of ceftriaxone, 1 g, is usually adequate systemic therapy. If there is corneal involvement, a 5-day course of parenteral ceftriaxone, 1-2 g daily, is required.
In acute purulent and mucopurulent conjunctivitis, the conjunctival sac should be irrigated with saline solution as necessary to remove the conjunctival secretions. To prevent spread of the disease, the patient and family should be instructed to give special attention to personal hygiene.
Course & Prognosis
Acute bacterial conjunctivitis is almost always self-limited. Untreated, it may last 10-14 days; if properly treated, 1-3 days. The exceptions are staphylococcal conjunctivitis (which may progress to blepharoconjunctivitis and enter a chronic phase) and gonococcal conjunctivitis (which when untreated can lead to corneal perforation and endophthalmitis). Since the conjunctiva may be the portal of entry for the meningococcus to the bloodstream and meninges, septicemia and meningitis may be the end results of meningococcal conjunctivitis.
Chronic bacterial conjunctivitis may not be self-limited and may become a troublesome therapeutic problem.
CHLAMYDIAL CONJUNCTIVITIS
1. TRACHOMA
Trachoma is one of the most ancient of known diseases. It was recognized as a cause of trichiasis as early as the 27th century BC and affects all races. With 300-600 million of the world's population afflicted, it is one of the most common of all chronic diseases. Its regional variations in prevalence and severity can be explained on the basis of variations in the personal hygiene and standards of living of the world's peoples, the climatic conditions under which they live, the prevailing age at onset, and the frequency and type of the prevailing concomitant bacterial eye infections. Blinding trachoma occurs in many parts of Africa, some parts of Asia, among Australian aborigines, and in northern Brazil. Communities with milder nonblinding trachoma occur in the same regions and in some areas of Latin America and the Pacific Islands.
Trachoma is usually bilateral. It is spread by direct contact or fomites, usually from other family members (siblings, parents), who should also be examined for the disease. Insect vectors, especially flies and gnats, may play a role in transmission. The acute forms of the disease are more infectious than the cicatricial forms, and the larger the inoculum the more severe the disease. Spread is often associated with epidemics of bacterial conjunctivitis and with the dry seasons in tropical and semitropical countries.
Clinical Findings
A. Symptoms and Signs:
Trachoma is initially a chronic follicular conjunctivitis of childhood that progresses to conjunctival scarring. In severe cases, inturned eyelashes occur in early adult life as a result of severe conjunctival scarring. The constant abrasion of inturned lashes and a defective tear film lead to corneal scarring, usually after the age of 50 years.
The incubation period of trachoma averages 7 days but varies from 5 to 14 days. In an infant or child, the onset is usually insidious, and the disease may resolve with minimal or no complications. In adults, the onset is often subacute or acute, and complications may develop early. At onset, trachoma often resembles other bacterial conjunctivitis, the signs and symptoms usually consisting of tearing, photophobia, pain, exudation, edema of the eyelids, chemosis of the bulbar conjunctiva, hyperemia, papillary hypertrophy, tarsal and limbal follicles, superior keratitis, pannus formation, and a small, tender preauricular node.
In established trachoma, there may also be superior epithelial keratitis, subepithelial keratitis, pannus, superior limbal follicles, and ultimately the pathognomonic cicatricial remains of these follicles, known as Herbert's pits-small depressions in the connective tissue at the limbocorneal junction covered by epithelium. The associated pannus is a fibrovascular membrane arising from the limbus, with vascular loops extending onto the cornea. All of the signs of trachoma are more severe in the upper than in the lower conjunctiva and cornea.
To establish the presence of endemic trachoma in a family or community, a substantial number of children must have at least two of the following signs:
Five or more follicles on the flat tarsal conjunctiva lining the upper eye lid.
Typical conjunctival scarring of the upper tarsal conjunctiva.
Limbal follicles or their sequelae (Herbert's pits).
An even extension of blood vessels onto the cornea, most marked at the upper limbus.
While occasional individuals will meet these criteria, it is the wide distribution of these signs in individual families and in a community that identify the presence of trachoma.
For control purposes, the World Health Organization has developed a simplified method to describe the disease. This includes the following signs:
| UNDEFINED: SIDEBARCONTENT | ||||
The presence of TF and TI indicates active infectious trachoma and a need for treatment. TS is evidence of damage from the disease. TT is potentially blinding and is an indication for corrective lid surgery. CO is the final blinding lesion of trachoma.
B. Laboratory Findings:
Chlamydial inclusions can be found in Giemsa-stained conjunctival scrapings, but they are not always present. Inclusions appear in the Giemsa-stained preparations as particulate, dark purple or blue cytoplasmic masses that cap the nucleus of the epithelial cell. Fluorescent antibody stains and enzyme immunoassay tests are available commercially and are widely used in clinical laboratories. These new tests have superseded Giemsa staining of conjunctival smears and isolation of chlamydial agent in cell culture.
The agent of trachoma resembles the agent of inclusion conjunctivitis morphologically, but the two can be differentiated serologically by microimmunofluorescence. Trachoma is caused by Chlamydia trachomatis serotypes A, B, Ba, or C.
Differential Diagnosis
Epidemiologic and clinical factors to be considered in differentiating trachoma from other forms of follicular conjunctivitis can be summarized as follows:
No history of exposure to endemic trachoma speaks against the diagnosis.
Viral follicular conjunctivitis (due to infection with adenovirus, herpes simplex virus, picornavirus, and coxsackievirus) usually has an acute onset and is clearly resolving by 2-3 weeks.
Infection with genitally transmitted chlamydial strains usually has an acute onset in sexually active individuals.
Chronic follicular conjunctivitis with exogenous substances (molluscum nodules of the lids, topical eye medications) resolve slowly when the nodules are removed or the drug withdrawn.
Parinaud's oculoglandular syndrome is manifested by massively enlarged preauricular or cervical lymph nodes, though the conjunctival lesion may be follicular.
Young children often have some follicles (like hypertrophied tonsils), a condition known as folliculosis.
The atopic conditions vernal conjunctivitis and atopic keratoconjunctivitis are associated with giant papillae that are elevated and often polygonal, with a milky-red appearance. Eosinophils are present in smears.
Look for a history of contact lens intolerance in patients with conjunctival scarring and pannus; giant papillae in some contact lens wearers can be confused with trachoma follicles.
Complications & Sequelae
Conjunctival scarring is a frequent complication of trachoma and can destroy the ductules of the accessory lacrimal glands and obliterate the orifices of the lacrimal gland. These effects may drastically reduce the aqueous component of the precorneal tear film, and the film's mucous components may be reduced by loss of goblet cells. The scars may also cause distortion of the upper lid with inward deviation of individual lashes (trichiasis) or of the whole lid margin (entropion), so that the lashes constantly abrade the cornea. This often leads to corneal ulceration, bacterial corneal infections, and corneal scarring (Figure 5-2).
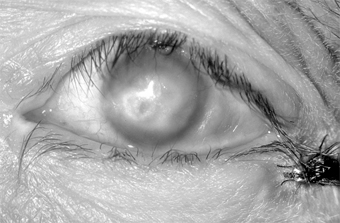
Figure 5-2: Advanced trachoma following corneal ulceration and scarring. Note the fly on the temporal aspect of the lower lid. The fly is a principal vector for trachoma.
Ptosis, nasolacrimal duct obstruction, and dacryocystitis are other common complications of trachoma.
Treatment
Striking clinical improvement can usually be achieved with tetracycline, 1-1.5 g/d orally in four divided doses for 3-4 weeks; doxycycline, 100 mg orally twice daily for 3 weeks; or erythromycin, 1 g/d orally in four divided doses for 3-4 weeks. Several courses are sometimes necessary for actual cure. Systemic tetracyclines should not be given to a child under 7 years of age or to a pregnant woman, since tetracycline binds to calcium in the developing teeth and in the growing bone and may lead to congenital yellowish discoloration of the permanent teeth and skeletal (eg, clavicular) abnormalities.
Topical ointments or drops, including preparations of sulfonamides, tetracyclines, erythromycin, and rifampin, used four times daily for 6 weeks, are equally effective.
From the time therapy is begun, its maximum effect is usually not achieved for 10-12 weeks. The persistence of follicles on the upper tarsus for some weeks after a course of therapy should therefore not be construed as evidence of therapeutic failure.
Surgical correction of inturned eyelashes is essential to prevent scarring from late trachoma in developing countries. Such surgery is sometimes done by nonspecialist physicians or specially trained auxiliary personnel.
Course & Prognosis
Characteristically, trachoma is a chronic disease of long duration. Under good hygienic conditions (specifically, face-washing of young children), the disease resolves or becomes milder so that severe sequelae are avoided. About 6-9 million people in the world today have major visual loss from trachoma.
2. INCLUSION CONJUNCTIVITIS
Inclusion conjunctivitis is often bilateral and usually occurs in sexually active young people. The chlamydial agent infects the urethra of the male and the cervix of the female. Transmission to the eyes of adults is usually by oral-genital sexual practices or hand to eye transmission. About one in 300 persons with genital chlamydial infection develops the eye disease. Indirect transmission has been reported to occur in inadequately chlorinated swimming pools. In newborns, the agent is transmitted during birth by direct contamination of the conjunctiva with cervical secretions. Credé prophylaxis gives only partial protection against inclusion conjunctivitis.
Clinical Findings
A. Symptoms and Signs:
Inclusion conjunctivitis may have an acute or a subacute onset. The patient frequently complains of redness of the eyes, pseudoptosis, and discharge, especially in the mornings. Newborns have papillary conjunctivitis and a moderate amount of exudate, and in hyperacute cases pseudomembranes occasionally form and can lead to scarring. Since the newborn has no adenoid tissue in the stroma of the conjunctiva, there is no follicle formation; but if the conjunctivitis persists for 2-3 months, follicles appear and the conjunctival picture is like that in older children and adults. In the newborn, chlamydial infection may cause pharyngitis, otitis media, and interstitial pneumonitis.
In adults, the conjunctiva of both tarsi-especially the lower tarsus-have papillae and follicles (Figure 5-3). Since pseudomembranes do not usually form in the adult, scarring does not usually occur. Superficial keratitis may be noted superiorly and, less often, a small superior micropannus (< 1-2 mm). Subepithelial opacities, usually marginal, often develop. Otitis media may occur as a result of infection of the auditory tube.

Figure 5-3: Acute follicular conjunctivitis caused by inclusion conjunctivitis in a 22-year-old man with urethritis. (Courtesy of K Tabbara.)
B. Laboratory Findings:
The same tests should be performed as for trachoma (above). In neonatal chlamydial ophthalmia, Giemsa-stained smears often have many inclusions. Inclusion conjunctivitis is caused by C trachomatis serotypes D-K with occasional isolations of serotype B. Serologic determinations are not useful in the diagnosis of ocular infections, but measurement of IgM antibody levels is extremely valuable in the diagnosis of chlamydial pneumonitis in infants.
Differential Diagnosis
Inclusion conjunctivitis can be clinically differentiated from trachoma on the following grounds:
Active, follicular trachoma occurs commonly in young children or others living in or exposed to a community with endemic trachoma; inclusion conjunctivitis occurs in sexually active adolescents or adults.
Conjunctival scarring is very rare in adult inclusion conjunctivitis.
Herbert's pits are a unique sign that trachoma was present at some time in the past.
Treatment
A. In Infants:
Give oral erythromycin suspension, 40 mg/kg/d in four divided doses for at least 14 days. Oral medication is necessary because chlamydial infection also involves the respiratory and gastrointestinal tracts. Topical antibiotics (tetracyclines, erythromycin, sulfonamides) are not useful in newborns treated with oral erythromycin. Both parents should be treated with oral tetracyclines or erythromycin for their genital tract infection.
B. In Adults:
Cure can be achieved with a 3-week course of oral tetracycline, 1-1.5 g/d; doxycycline, 100 mg orally twice daily; or erythromycin, 1 g/d. (Systemic tetracyclines should not be given to a pregnant woman or a child under 7 years of age, since they cause epiphysial problems in the fetus or staining of the young child's teeth.) The patient's sexual partners should be examined and treated.
When one of the standard therapeutic regimens is followed, recurrences are rare. If untreated, inclusion conjunctivitis runs a course of 3-9 months or longer. The average duration is 5 months.
3. CONJUNCTIVITIS CAUSED BY OTHER CHLAMYDIAL AGENTS
Lymphogranuloma venereum conjunctivitis is a rare sexually transmitted disease. Lymphogranuloma venereum causes a dramatic granulomatous conjunctival reaction with greatly enlarged preauricular nodes (Parinaud's syndrome). It is caused by C trachomatis serotypes L1, L2 or L3.
Chlamydia psittaci only rarely causes conjunctivitis in humans. Strains from parrots (psittacosis) and cats (feline pneumonitis) have caused follicular conjunctivitis in humans. The prototype strains of Chlamydia pneumoniae were isolated from the conjunctiva but have not been identified as a cause of eye disease.
VIRAL CONJUNCTIVITIS
Viral conjunctivitis, a common affliction, can be caused by a wide variety of viruses. Severity ranges from severe, disabling disease to mild, rapidly self-limited infection.
1. ACUTE VIRAL FOLLICULAR CONJUNCTIVITIS
Pharyngoconjunctival Fever
Pharyngoconjunctival fever is characterized by fever of 38.3-40 °C (101-104 °F), sore throat, and a follicular conjunctivitis in one or both eyes. The follicles are often very prominent on both the conjunctiva (Figure 5-4) and the pharyngeal mucosa. The disease can be either bilateral or unilateral. Injection and tearing often occur, and there may be transient superficial epithelial keratitis and occasionally some subepithelial opacities. Preauricular lymphadenopathy (nontender) is characteristic. The syndrome may be incomplete, consisting of only one or two of the cardinal signs (fever, pharyngitis, and conjunctivitis).
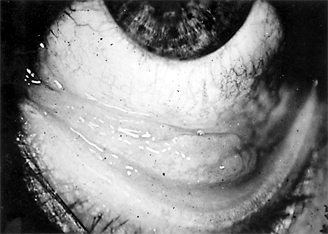
Figure 5-4: Acute follicular conjunctivitis due to adenovirus type 3. (Courtesy of P Thygeson.)
Pharyngoconjunctival fever is caused regularly by adenovirus type 3 and occasionally by types 4 and 7. The virus can be grown on HeLa cells and identified by neutralization tests. As the disease progresses, it can also be diagnosed serologically by a rising titer of neutralizing antibody to the virus. Clinical diagnosis is a simple matter, however, and clearly more practical.
Conjunctival scrapings contain predominantly mononuclear cells, and no bacteria grow in cultures. The condition is more common in children than in adults and can be transmitted poorly in chlorinated swimming pools. There is no specific treatment, but the conjunctivitis is self-limited, usually lasting about 10 days.
Epidemic Keratoconjunctivitis
Epidemic keratoconjunctivitis is usually bilateral. The onset is often in one eye only, however, and as a rule the first eye is more severely affected. At onset the patient notes injection, moderate pain, and tearing, followed in 5-14 days by photophobia, epithelial keratitis, and round subepithelial opacities. Corneal sensation is normal. A tender preauricular node is characteristic. Edema of the eyelids, chemosis, and conjunctival hyperemia mark the acute phase, with follicles and subconjunctival hemorrhages often appearing within 48 hours. Pseudomembranes (and occasionally true membranes) may occur and may be followed by flat scars or symblepharon formation (Figure 5-5).
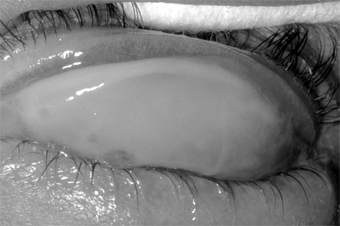
Figure 5-5: Epidemic keratoconjunctivitis. Thick white membrane of upper palpebral conjunctiva.
The conjunctivitis lasts for 3-4 weeks at most. The subepithelial opacities are concentrated in the central cornea, usually sparing the periphery, and may persist for months but heal without scars.
Epidemic keratoconjunctivitis is caused by adenovirus types 8, 19, 29, and 37 (subgroup D of the human adenoviruses). They can be isolated in cell culture and identified by neutralization tests. Scrapings from the conjunctiva show a primarily mononuclear inflammatory reaction (Figure 5-6); when pseudomembranes occur, neutrophils may also be prominent.
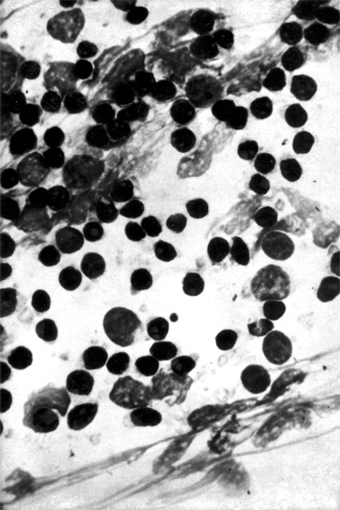
Figure 5-6: Mononuclear cell reaction in conjunctival scrapings of a patient with viral conjunctivitis caused by adenovirus type 8. (Courtesy of M Okumoto.)
Epidemic keratoconjunctivitis in adults is confined to the external eye, but in children there may be such systemic symptoms of viral infection as fever, sore throat, otitis media, and diarrhea. Nosocomial transmission during eye examinations takes place all too often by way of the physician's fingers, use of improperly sterilized ophthalmic instruments, or use of contaminated solutions. Eye solutions, particularly topical anesthetics, can be contaminated when a dropper tip aspirates infected material from the conjunctiva or cilia. The virus can persist in the solution, which becomes a source of spread.
The danger of contaminated solution bottles can be avoided by the use of individual sterile droppers or unit-dose packages of eye drops. Regular hand washing between examinations and careful cleaning and sterilization of instruments that touch the eyes-especially tonometers-are also mandatory. Applanation tonometers should be cleaned by wiping with alcohol or hypochlorite, then rinsing with sterile water and carefully drying.
There is no specific therapy at present, but cold compresses will relieve some symptoms. Corticosteroids during acute conjunctivitis may prolong the late corneal involvement and so should be avoided. Antibacterial agents should be given if bacterial superinfection occurs.
Herpes Simplex Virus Conjunctivitis
Herpes simplex virus (HSV) conjunctivitis, usually a disease of young children, is an uncommon entity characterized by unilateral injection, irritation, mucoid discharge, pain, and mild photophobia. It occurs during primary infection with HSV or during recurrent episodes of ocular herpes (Figure 5-7). It is often associated with herpes simplex keratitis, in which the cornea shows discrete epithelial lesions that usually coalesce to form single or multiple branching epithelial (dendritic) ulcers. The conjunctivitis is follicular or, less often, pseudomembranous. (Patients receiving topical antivirals may develop follicular conjunctivitis that can be differentiated because the herpetic follicular conjunctivitis has an acute onset.) Herpetic vesicles may sometimes appear on the eyelids and lid margins, associated with severe edema of the eyelids. Typically, there is a small tender preauricular node.

Figure 5-7: Primary ocular herpes. (Courtesy of HB Ostler.)
No bacteria are found in scrapings or recovered in cultures. If the conjunctivitis is follicular, the predominant inflammatory reaction is mononuclear, but if it is pseudomembranous the predominant reaction is polymorphonuclear owing to the chemotaxis of necrosis. Intranuclear inclusions (because of the margination of the chromatin) can be seen in conjunctival and corneal cells if Bouin fixation and the Papanicolaou stain are used but not in Giemsa-stained smears. The finding of multinucleated giant epithelial cells has diagnostic value.
The virus can be readily isolated by gently rubbing a dry cotton-tipped applicator over the conjunctiva and transferring the infected cells to a susceptible tissue culture.
HSV conjunctivitis may persist for 2-3 weeks, and if it is pseudomembranous it may leave fine linear or flat scars. Complications consist of corneal involvement (including dendrites) and vesicles on the skin. Although type 1 herpesvirus causes the overwhelming majority of ocular cases, type 2 is the usual cause in newborns and a rare cause in adults. In the newborn, there may be generalized disease with encephalitis, chorioretinitis, hepatitis, etc. Any HSV infection in the newborn must be treated with systemic antiviral therapy (acyclovir) and monitored in a hospital setting.
If the conjunctivitis occurs in a child over 1 year of age or in an adult, it is usually self-limited and may not require therapy. Topical or systemic antivirals should be given, however, to prevent corneal involvement. For corneal ulcers, corneal debridement may be performed by gently wiping the ulcer with a dry cotton swab, applying antiviral drops, and patching the eye for 24 hours. Topical antivirals alone should be applied for 7-10 days: trifluridine every 2 hours while awake, or vidarabine ointment five times a day, or idoxuridine 0.1%, 1 drop every hour while awake and 1 drop every 2 hours during the night. Herpetic keratitis may also be treated with 3% acyclovir ointment (not available in the USA) five times daily for 10 days or with oral acyclovir, 400 mg five times a day for 7 days. The use of steroids is contraindicated, since they may aggravate herpes simplex infections and convert the disease from a short, self-limited process to a severe, greatly prolonged one.
Newcastle Disease Conjunctivitis
Newcastle disease conjunctivitis is a rare disorder characterized by burning, itching, pain, redness, tearing, and (rarely) blurring of vision. It often occurs in small epidemics among poultry workers handling infected birds or among veterinarians or laboratory helpers working with live vaccines or virus.
The conjunctivitis resembles that caused by other viral agents, with chemosis, a small preauricular node, and follicles on the upper and lower tarsus. No treatment is available or necessary for this self-limited disease.
Acute Hemorrhagic Conjunctivitis
All of the continents and most of the islands of the world have had major epidemics of acute hemorrhagic conjunctivitis. It was first recognized in Ghana in 1969. It is caused by enterovirus type 70 and occasionally by coxsackievirus A24.
Characteristically, the disease has a short incubation period (8-48 hours) and course (5-7 days). The usual signs and symptoms are pain, photophobia, foreign body sensation, copious tearing, redness, lid edema, and subconjunctival hemorrhages (Figure 5-8). Chemosis sometimes also occurs. The subconjunctival hemorrhages are usually diffuse but may be punctate at onset, beginning in the upper bulbar conjunctiva and spreading to the lower. Most patients have preauricular lymphadenopathy, conjunctival follicles, and epithelial keratitis. Anterior uveitis has been reported; fever, malaise, and generalized myalgia have been observed in 25% of cases; and motor paralysis of the lower extremities has occurred in rare cases in India and Japan.
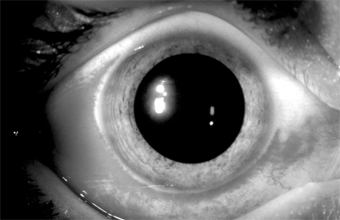
Figure 5-8: Acute hemorrhagic conjunctivitis.
The virus is transmitted by close person-to-person contact and by such fomites as common linens, contaminated optical instruments, and water. Recovery occurs within 5-7 days, and there is no known treatment. In the USA, closing of schools has been done to stop epidemics.
2. CHRONIC VIRAL CONJUNCTIVITIS
Molluscum Contagiosum Blepharoconjunctivitis
A molluscum nodule on the lid margins or the skin of the lids or brow may produce unilateral chronic follicular conjunctivitis, superior keratitis, and superior pannus and may resemble trachoma. The inflammatory reaction is predominantly mononuclear (unlike the reaction in trachoma), and the round, waxy, pearly-white, noninflammatory lesion with an umbilicated center is typical of molluscum contagiosum (Figure 5-9). Biopsy shows eosinophilic cytoplasmic inclusions that fill the entire cytoplasm of the enlarged cell, pushing its nucleus to one side.

Figure 5-9: Molluscum contagiosum of lid margin. Follicular conjunctivitis was present.
Excision, simple incision of the nodule to allow peripheral blood to permeate it, or cryotherapy cures the conjunctivitis. On very rare occasions (reports of only two cases have appeared in the literature), molluscum nodules have occurred on the conjunctiva. In these cases, excision of the nodule has also relieved the conjunctivitis. Multiple lid or facial lesions of molluscum contagiosum have been seen in patients with acquired immune deficiency syndrome (AIDS).
Varicella-Zoster Blepharoconjunctivitis
Hyperemia and an infiltrative conjunctivitis-associated with the typical vesicular eruption along the dermatomal distribution of the ophthalmic branch of the trigeminal nerve-are characteristic of herpes zoster (preferably called simply zoster). The conjunctivitis is usually papillary, but follicles, pseudomembranes, and transitory vesicles that later ulcerate have all been noted. A tender preauricular lymph node occurs early in the disease. Scarring of the lid, entropion, and the misdirection of individual lashes are sequelae.
The lid lesions of varicella, which are like the skin lesions (pox) elsewhere, may appear on both the lid margins and the lids and often leave scars. A mild exudative conjunctivitis often occurs, but discrete conjunctival lesions (except at the limbus) are very rare. Limbal lesions resemble phlyctenules and may go through all the stages of vesicle, papule, and ulcer. The adjacent cornea becomes infiltrated and may vascularize.
In both zoster and varicella, scrapings from lid vesicles contain giant cells and a predominance of polymorphonuclear leukocytes; scrapings from the conjunctiva in varicella and from conjunctival vesicles in zoster may contain giant cells and monocytes. The virus can be recovered in tissue cultures of human embryo cells.
Oral acyclovir in high doses (800 mg orally five times daily for 10 days), if given early in the course of the disease, appears to limit the severity of the illness.
Measles Keratoconjunctivitis
The characteristic enanthem of measles frequently precedes the skin eruption. At this early stage, the conjunctiva may have a peculiar glassy appearance, followed within a few days by swelling of the semilunar fold (Meyer's sign). Several days before the skin eruption, an exudative conjunctivitis with a mucopurulent discharge develops, and at the time of the skin eruption, Koplik's spots appear on the conjunctiva and occasionally on the caruncle. At some time (early in children, late in adults), epithelial keratitis supervenes.
In the immunocompetent patient, measles keratoconjunctivitis has few or no sequelae, but in malnourished or otherwise immunoincompetent patients the ocular disease is frequently associated with a secondary HSV or bacterial infection due to S pneumoniae, H influenzae, and other organisms. These agents may lead to purulent conjunctivitis with associated corneal ulceration and severe visual loss. Herpes infection can cause severe corneal ulceration with corneal perforation and loss of vision in poorly nourished children in developing countries.
Conjunctival scrapings show a mononuclear cell reaction unless there are pseudomembranes or secondary infection. Giemsa-stained preparations contain giant cells. Since there is no specific therapy, only supportive measures are indicated unless there is secondary infection.
RICKETTSIAL CONJUNCTIVITIS
All rickettsiae recognized as pathogenic for humans may attack the conjunctiva, and the conjunctiva may be their portal of entry.
Q fever is associated with severe conjunctival hyperemia. Treatment with systemic tetracycline or chloramphenicol is curative.
Marseilles fever (boutonneuse fever) is often associated with ulcerative or granulomatous conjunctivitis and a grossly visible preauricular lymph node.
Endemic (murine) typhus, scrub typhus, Rocky Mountain spotted fever, and epidemic typhus have associated, variable, and usually mild conjunctival signs.
FUNGAL CONJUNCTIVITIS
Candidal Conjunctivitis
Conjunctivitis caused by Candida species (usually Candida albicans) is a rare infection that usually appears as a white plaque. This may occur in diabetics or immunocompromised patients as an ulcerative or granulomatous conjunctivitis.
Scrapings show a polymorphonuclear cell inflammatory reaction. The organism grows readily on blood agar or Sabouraud's medium and can be readily identified as a budding yeast or, rarely, as pseudohyphae.
The infection responds to amphotericin B (3-8 mg/mL) in aqueous (not saline) solution or to applications of nystatin dermatologic cream (100,000 units/g) four to six times daily. The ointment must be applied carefully to be sure that it reaches the conjunctival sac and does not just build up on the lid margins.
Other Fungal Conjunctivitides
Sporothrix schenckii may rarely involve the conjunctiva or the eyelids. It is a granulomatous disease associated with a visible preauricular node. Microscopic examination of a biopsy of the granuloma reveals gram-positive, cigar-shaped conidia (spores).
Rhinosporidium seeberi may rarely affect the conjunctiva, lacrimal sac, lids, canaliculi, and sclera. The typical lesion is a polypoid granuloma that bleeds after minimal trauma. Histologic examination shows a granuloma with enclosed large spherules containing myriads of endospores. Treatment is by simple excision and cauterization of the base.
Coccidioides immitis may rarely cause a granulomatous conjunctivitis associated with a grossly visible preauricular node (Parinaud's oculoglandular syndrome). This is not a primary disease but a manifestation of metastatic infection from a primary pulmonary infection (San Joaquin Valley fever). Disseminated disease suggests a poor prognosis.
PARASITIC CONJUNCTIVITIS*
Thelazia californiensis Infection
The natural habitat of this roundworm is the eye of the dog, but it can also infect the eyes of cats, sheep, black bears, horses, and deer. Accidental infection of the human conjunctival sac has occurred. The disease can be treated effectively by removing the worms from the conjunctival sac with forceps or a cotton-tipped applicator.
Loa loa Infection
L loa is the eye worm of Africa. It lives in the connective tissue of humans and monkeys, and the monkey may be its reservoir. The parasite is transmitted by the bite of the horse or mango fly. The mature worm may then migrate to the lid, the conjunctiva, or the orbit.
Infection with L loa is accompanied by a 60-80% eosinophilia, but diagnosis is made by identifying the worm on removal or by finding microfilariae in blood examined at midday.
Diethylcarbamazine is currently the drug of choice. Ivermectin is being evaluated.
Ascaris lumbricoides Infection (Butcher's Conjunctivitis)
Ascaris may cause a rare type of violent conjunctivitis. When butchers or persons performing postmortem examinations cut tissue containing Ascaris, the tissue juice of some of the organisms may hit them in the eye. This can be followed by a violent and painful toxic conjunctivitis marked by extreme chemosis and lid edema. Treatment consists of rapid and thorough irrigation of the conjunctival sac.
Trichinella spiralis Infection
This parasite does not cause a true conjunctivitis, but in the course of its general dissemination there may be a doughy edema of the upper and lower eyelids, and over 50% of patients have chemosis-a pale, lemon-yellow swelling most marked over the lateral and medial rectus muscles and fading toward the limbus. The chemosis may last a week or more, and there is often pain on movement of the eyes.
Schistosoma haematobium Infection
Schistosomiasis (bilharziasis) is endemic in Egypt, especially in the region irrigated by the Nile. Granulomatous conjunctival lesions appearing as small, soft, smooth, pinkish-yellow tumors occur, especially in males. The symptoms are minimal. Diagnosis depends on microscopic examination of biopsy material, which shows a granuloma containing lymphocytes, plasma cells, giant cells, and eosinophils surrounding bilharzial ova in various stages of disintegration.
Treatment consists of excision of the conjunctival granuloma and systemic therapy with antimonials such as niridazole.
Taenia solium Infection
This parasite rarely causes conjunctivitis but more often invades the retina, choroid, or vitreous to produce ocular cysticercosis. As a rule, the affected conjunctiva shows a subconjunctival cyst in the form of a localized hemispherical swelling, usually at the inner angle of the lower fornix, which is adherent to the underlying sclera and painful on pressure. The conjunctiva and lid may be inflamed and edematous.
Diagnosis is based on a positive complement fixation or precipitin test or on demonstration of the organism in the gastrointestinal tract. Eosinophilia is a constant feature.
The best treatment is to excise the lesion. The intestinal condition can be treated by niclosamide.
Pthirus pubis Infection (Pubic Louse Infection)
P pubis may infest the cilia and margins of the eyelids. Because of its size, the pubic louse seems to require widely spaced hair. For this reason it has a predilection for the widely spaced cilia as well as for pubic hair. The parasites apparently release an irritating substance (probably feces) that produces a toxic follicular conjunctivitis in children and an irritating papillary conjunctivitis in adults. The lid margin is usually red, and the patient may complain of intense itching.
Finding the adult organism or the ova-shaped nits cemented to the eyelashes is diagnostic.
Lindane (Kwell) 1% or RID (pyrethrins), applied to the pubic area and lash margins after removal of the nits, is usually curative. Application of lindane or RID to the lid margins must be undertaken with great care to avoid contact with the eye. Any ointment applied to the lid margin tends to smother the adult organisms. The patient's family and close contacts should be examined and treated. All clothes and fomites should be washed.
Ophthalmomyiasis
Myiasis is infection with larvae of flies. Many different species of flies may produce myiasis. The ocular tissues may be injured by mechanical transmission of disease-producing organisms and by the parasitic activities of the larvae in the ocular tissues. The larvae are able to invade either necrotic or healthy tissue. Many become infected by accidental ingestion of the eggs or larvae or by contamination of external wounds or skin. Infants and young children, alcoholics, and debilitated unattended patients are common targets for infection with myiasis-producing flies.
These larvae may affect the ocular surface, the intraocular tissues, or the deeper orbital tissues.
Ocular surface involvement may be caused by Musca domestica, the housefly, Fannia, the latrine fly, and Oestrus ovis, the sheep botfly. These flies deposit their eggs at the lower lid margin or inner canthus, and the larvae may remain on the surface of the eye, causing irritation, pain, and conjunctival hyperemia.
Treatment of ocular surface myiasis is by mechanical removal of the larvae after topical anesthesia.
** Onchocerciasis is discussed in Chapter 7
IMMUNOLOGIC (ALLERGIC) CONJUNCTIVITIS
IMMEDIATE HUMORAL HYPERSENSITIVITY REACTIONS
1. HAY FEVER CONJUNCTIVITIS
A mild, nonspecific conjunctival inflammation is commonly associated with hay fever (allergic rhinitis). There is usually a history of allergy to pollens, grasses, animal danders, etc. The patient complains of itching, tearing, and redness of the eyes and often states that the eyes seem to be "sinking into the surrounding tissue." There is mild injection of the palpebral and bulbar conjunctiva, and during acute attacks there is often severe chemosis (which no doubt accounts for the "sinking" description). There may be a small amount of ropy discharge, especially if the patient has been rubbing the eyes. Eosinophils are difficult to find in conjunctival scrapings. A papillary conjunctivitis can occur if the allergen persists (Figure 5-10).

Figure 5-10: Acute hypersensitivity with moderate tylosis, moderate to marked chemosis and mild injection of the conjunctiva. Note that the eye seems to be "sinking" into the surrounding tissue.
Treatment consists of the instillation of local vasoconstrictors during the acute phase (epinephrine, 1:1000 solution applied topically, will relieve the chemosis and symptoms within 30 minutes). Cold compresses are helpful to relieve itching, and antihistamines by mouth are of some value. The immediate response to treatment is satisfactory, but recurrences are common unless the antigen is eliminated. Fortunately, the frequency of the attacks and the severity of the symptoms tend to moderate as the patient ages.
2. VERNAL KERATOCONJUNCTIVITIS
This disease, also known as "spring catarrh" and "seasonal conjunctivitis" or "warm weather conjunctivitis," is an uncommon bilateral allergic disease that usually begins in the prepubertal years and lasts for 5-10 years. It occurs much oftener in boys than in girls. The specific allergen or allergens are difficult to identify, but patients with vernal keratoconjunctivitis usually show other manifestations of allergy known to be related to grass pollen sensitivity. The disease is less common in temperate than in warm climates and is almost nonexistent in cold climates. It is almost always more severe during the spring, summer, and fall than in the winter. It is most commonly seen in sub-Saharan Africa and the Middle East.
The patient usually complains of extreme itching and a ropy discharge. There is often a family history of allergy (hay fever, eczema, etc) and sometimes in the young patient as well. The conjunctiva has a milky appearance, and there are many fine papillae in the lower tarsal conjunctiva. The upper palpebral conjunctiva often has giant papillae that give a cobblestone appearance (Figure 5-11). Each giant papilla is polygonal, has a flat top, and contains tufts of capillaries.
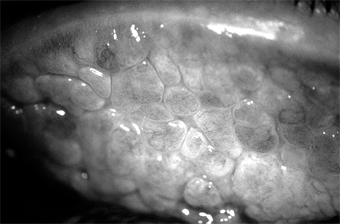
Figure 5-11: Vernal keratoconjunctivitis. "Cobblestone" papillae on superior tarsal conjunctiva.
A stringy conjunctival discharge and a fine, fibrinous pseudomembrane (Maxwell-Lyons sign) may be noted, especially on the upper tarsus on exposure to heat. In some cases, especially in persons of black African ancestry, the most prominent lesions are located at the limbus, where gelatinous swellings (papillae) are noted. A pseudogerontoxon (arcus-like haze) is often noted in the cornea adjacent to the limbal papillae. Trantas' dots are whitish dots seen at the limbus in some patients with vernal keratoconjunctivitis during the active phase of the disease. Many eosinophils and free eosinophilic granules are found in Giemsa-stained smears of the conjunctival exudate and in Trantas' dots.
Micropannus is often seen in both palpebral and limbal vernal keratoconjunctivitis, but gross pannus is unusual. Conjunctival scarring usually does not occur unless the patient has been treated with cryotherapy, surgical removal of the papillae, irradiation, or other damaging procedure. Superficial corneal ("shield") ulcers (oval and located superiorly) may form and may be followed by mild corneal scarring. A characteristic diffuse epithelial keratitis frequently occurs. None of the corneal lesions respond well to standard treatment.
The disease may be associated with keratoconus.
Treatment
Since vernal keratoconjunctivitis is a self-limited disease, it must be recognized that the medication used to treat the symptoms may provide short-term benefit but long-term harm. Topical and systemic steroids, which relieve the itching, affect the corneal disease only minimally, and their side effects (glaucoma, cataract, and other complications) can be severely damaging. Topical cromolyn is a useful prophylactic agent in moderate to severe cases. Vasoconstrictors, cold compresses, and ice packs are helpful, and sleeping (if possible, also working) in cool, air-conditioned rooms can keep the patient reasonably comfortable. Probably the best remedy of all is to move to a cool, moist climate. Patients able to do so are benefited if not completely cured.
The severe symptoms of an extremely photophobic patient who is unable to function can often be relieved by a short course of topical or systemic steroids followed by vasoconstrictors, cold packs, and regular use of histamine-blocking agents as eyedrops. Newer nonsteroidal anti-inflammatory medications, including ketorolac and lodoxamide, may provide significant symptomatic relief. (See discussion in Chapter 3.) As has already been indicated, the prolonged use of steroids must be avoided since it is all too often followed by herpes simplex keratitis, cataract, glaucoma, and fungal and other opportunistic corneal ulcers. Recent clinical studies have shown that topical 2% cyclosporine eye drops are effective in severe unresponsive cases. Supratarsal injection of depot corticosteroids has been demonstrated to be effective for vernal shield ulcers.
Desensitization to grass pollens and other antigens has not been rewarding. Staphylococcal blepharitis and conjunctivitis are frequent complications and should be treated. Recurrences are the rule, particularly in the spring and summer; but after a number of recurrences the papillae disappear completely, leaving no scars.
3. ATOPIC KERATOCONJUNCTIVITIS
Patients with atopic dermatitis (eczema) often also have atopic keratoconjunctivitis. The symptoms and signs are a burning sensation, mucoid discharge, redness, and photophobia. The lid margins are erythematous, and the conjunctiva has a milky appearance. There are fine papillae, but giant papillae are less developed than in vernal keratoconjunctivitis and occur more frequently on the lower tarsus-unlike the giant papillae of vernal keratoconjunctivitis, which are on the upper tarsus (Figure 5-12). Severe corneal signs appear late in the disease after repeated exacerbations of the conjunctivitis. Superficial peripheral keratitis develops and is followed by vascularization. In severe cases, the entire cornea becomes hazy and vascularized, and visual acuity is reduced. The disease may be associated with keratoconus.
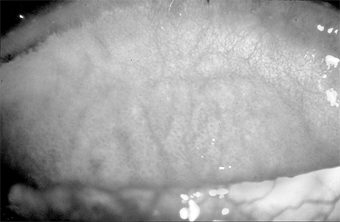
Figure 5-12: Moderate to marked papillary response of upper tarsus seen in atopic keratoconjunctivitis.
There is usually a history of allergy (hay fever, asthma, or eczema) in the patient or the patient's family. Most patients have had atopic dermatitis since infancy. Scarring of the flexure creases of the antecubital folds and of the wrists and knees is common. Like the dermatitis with which it is associated, atopic keratoconjunctivitis has a protracted course and is subject to exacerbations and remissions. Like vernal keratoconjunctivitis, it tends to become less active when the patient reaches the fifth decade.
Scrapings of the conjunctiva show eosinophils, though not nearly as many as are seen in vernal keratoconjunctivitis. Scarring of both the conjunctiva and cornea is often seen, and an atopic cataract, a posterior subcapsular plaque, or an anterior shield-like cataract may develop. Keratoconus, retinal detachment, and herpes simplex keratitis are all more than usually frequent in patients with atopic keratoconjunctivitis, and there are many cases of secondary bacterial blepharitis and conjunctivitis, usually staphylococcal.
The management of atopic keratoconjunctivitis is often discouraging. Any secondary infection must be treated. Environmental control should be considered. Oral antihistamines including terfenadine (60-120 mg twice daily), astemizole (10 mg four times daily), or hydroxyzine (50 mg at bedtime, increasing to 200 mg at bedtime) have been shown to be of value. Newer nonsteroidal anti-inflammatory medications, including ketorolac and lodoxamide, show promise for symptomatic relief for these patients (see Chapter 3). A short course of topical steroids may relieve symptoms. In severe cases, plasmapheresis may be an adjunct to therapy. In advanced cases with severe corneal complications, corneal transplantation may be needed to improve the visual acuity.
4. GIANT PAPILLARY CONJUNCTIVITIS
Giant papillary conjunctivitis with signs and symptoms resembling those of vernal conjunctivitis may develop in patients wearing plastic artificial eyes or contact lenses. It is probably a basophil-rich delayed hypersensitivity disorder (Jones-Mote hypersensitivity), perhaps with an IgE humoral component. Use of glass instead of plastic for prostheses and spectacle lenses instead of contact lenses is curative. If the goal is to maintain contact lens wear, additional therapy will be required. Careful contact lens care, including preservative-free agents, is essential. Hydrogen peroxide disinfection and enzymatic cleaning of contact lenses may also help. Changing to a different brand or style of contact lenses may be necessary if other measures fail. If these treatments are unsuccessful, contact lenses should be discontinued.
DELAYED HYPERSENSITIVITY REACTIONS
1. PHLYCTENULOSIS
Phlyctenular keratoconjunctivitis is a delayed hypersensitivity response to microbial proteins, including the proteins of the tubercle bacillus, Staphylococcus species, Candida albicans, Coccidioides immitis, Haemophilus aegyptius, and Chlamydia trachomatis serotypes L1, L2, and L3. Until recently, by far the most frequent cause of phlyctenulosis in the USA was delayed hypersensitivity to the protein of the human tubercle bacillus. This is still the commonest cause in regions where tuberculosis is still prevalent. In the USA, however, most cases are now associated with delayed hypersensitivity to S aureus.
The conjunctival phlyctenule begins as a small lesion (usually 1-3 mm in diameter) that is hard, red, elevated, and surrounded by a zone of hyperemia. At the limbus it is often triangular in shape, with its apex toward the cornea. In this location it develops a grayish-white center that soon ulcerates and then subsides within 10-12 days. The patient's first phlyctenule and most of the recurrences develop at the limbus, but there may also be corneal, bulbar, and, very rarely, even tarsal phlyctenules.
Unlike the conjunctival phlyctenule, which leaves no scar, the corneal phlyctenule develops as an amorphous gray infiltrate and always leaves a scar. Consistent with this difference is the fact that scars form on the corneal side of the limbal lesion and not on the conjunctival side. The result is a triangular scar with its base at the limbus-a valuable sign of old phlyctenulosis when the limbus has been involved.
Conjunctival phlyctenules usually produce only irritation and tearing, but corneal and limbal phlyctenules are usually accompanied by intense photophobia (Figure 5-13). Phlyctenulosis is often triggered by active blepharitis, acute bacterial conjunctivitis, and dietary deficiencies. Phlyctenular scarring, which may be minimal or extensive, is often followed by Salzmann's nodular degeneration.
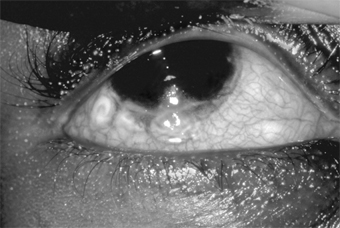
Figure 5-13: Phlyctenulosis. Note three phlyctenules along the inferior limbus, each with an umbilicated center.
Histologically, the phlyctenule is a focal subepithelial and perivascular infiltration of small round cells, followed by a preponderance of polymorphonuclear cells when the overlying epithelium necrotizes and sloughs-a sequence of events characteristic of the delayed tuberculin type hypersensitivity reaction.
Phlyctenulosis induced by tuberculoprotein and the proteins of other systemic infections responds dramatically to topical corticosteroids. There is a major reduction of symptoms within 24 hours and disappearance of the lesion in another 24 hours. Phlyctenulosis produced by staphylococcal proteins responds somewhat more slowly. Topical antibiotics should be added for active staphylococcal blepharoconjunctivitis. Treatment should be aimed at the underlying disease, and the steroids, when effective, should be used only to control acute symptoms and persistent corneal scarring. Severe corneal scarring may call for corneal transplantation.
2. MILD CONJUNCTIVITIS SECONDARY TO CONTACT BLEPHARITIS
Contact blepharitis caused by atropine, neomycin, broad-spectrum antibiotics, and other topically applied medications is often followed by a mild infiltrative conjunctivitis that produces hyperemia, mild papillary hypertrophy, a mild mucoid discharge, and some irritation (Figure 5-14). Examination of Giemsa-stained scrapings often discloses only a few degenerated epithelial cells, a few polymorphonuclear and mononuclear cells, and no eosinophils.
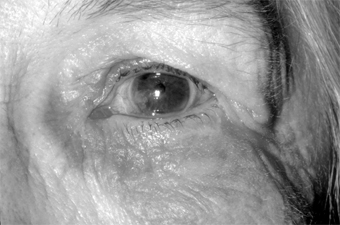
Figure 5-14: Contact dermatitis secondary to neomycin. Note lower lid involvement.
Treatment should be directed toward finding the offending agent and eliminating it. The contact blepharitis may clear rapidly with topical cortico-steroids, but their use should be limited. Long-term use of steroids on the lids may lead to steroid glaucoma and to skin atrophy with disfiguring telangiectasis.
CONJUNCTIVITIS DUE TO AUTOIMMUNE DISEASE
KERATOCONJUNCTIVITIS SICCA (ASSOCIATED WITH SJÖGREN'S SYNDROME)
Sjögren's syndrome is a systemic disease characterized by a triad of disorders: keratoconjunctivitis sicca, xerostomia, and connective tissue dysfunction (arthritis). To establish the diagnosis of Sjögren's syndrome, at least two of the three disorders must be present. The disease is overwhelmingly more common in women at or beyond the menopause than in other groups, though men and younger women can also be affected. The lacrimal gland is infiltrated with lymphocytes and occasionally with plasma cells, and this leads to atrophy and destruction of the glandular structures.
Keratoconjunctivitis sicca is characterized by bulbar conjunctival hyperemia (especially in the palpebral aperture) and symptoms of irritation that are out of proportion to the mild inflammatory signs. It often begins as a mild conjunctivitis with a mucoid discharge. Blotchy epithelial lesions appear on the cornea, more prominently in its lower half, and filaments may be seen. Pain builds up in the afternoon and evening but is absent or only slight in the morning. The tear film is diminished and often contains shreds of mucus. Results of the Schirmer test are abnormal (see Chapter 4). Rose bengal or lissamine green staining of the cornea and conjunctiva in the palpebral aperture is a helpful diagnostic test.
The diagnosis is confirmed by demonstrating lymphocytic and plasma cell infiltration of the accessory salivary glands in a labial biopsy obtained by means of a simple surgical procedure (Figure 5-15).
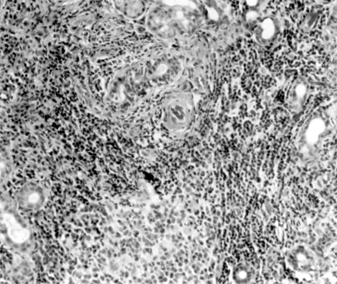
Figure 5-15: Mononuclear infiltration of the accessory salivary glands of a patient with Sjögren's syndrome. (Courtesy of K Tabbara.)
Treatment should be directed toward preserving and replacing the tear film with artificial tears, with obliteration of the puncta, and with side shields, moisture chambers, and Buller shields. As a rule, the simpler measures should be tried first.
CICATRICIAL PEMPHIGOID
This disease usually begins as a nonspecific chronic conjunctivitis that is resistant to therapy. The conjunctiva may be affected alone or in combination with the mouth, nose, esophagus, vulva, and skin. The conjunctivitis leads to progressive scarring, obliteration of the fornices (especially the lower fornix), and entropion with trichiasis. The patient complains of pain, irritation, and blurring of vision. The cornea is affected only secondarily as a result of trichiasis and lack of the precorneal tear film. The disease is more severe in women than in men. It is typically a disease of middle life, occurring very rarely before age 45. In women, it may progress to blindness in a year or less; in men, progress is slower, and spontaneous remission sometimes occurs.
Conjunctival biopsies may contain eosinophils, and the basement membrane will stain positively with certain immunofluorescent stains (IgG, IgM, IgA complement). Oral dapsone and immunosuppressive therapy (eg, sulfapyridine) have been effective in some cases. Treatment must always be instituted at an early stage, prior to the onset of significant scarring. Generally, the course is long and the prognosis poor, with blindness due to complete symblepharon and corneal desiccation the usual outcome.
CHEMICAL OR IRRITATIVE CONJUNCTIVITIS
IATROGENIC CONJUNCTIVITIS FROM TOPICALLY APPLIED DRUGS
A toxic follicular conjunctivitis or an infiltrative, nonspecific conjunctivitis, followed by scarring, is often produced by the prolonged administration of dipivefrin, miotics, idoxuridine, neomycin, and other drugs prepared in toxic or irritating preservatives or vehicles. Silver nitrate instilled into the conjunctival sac at birth (Credé prophylaxis) is a frequent cause of mild chemical conjunctivitis. If tear production is reduced by continual irritation, the conjunctiva can be further damaged by the lack of dilution of the noxious agent as it is instilled into the conjunctival sac.
Conjunctival scrapings often contain keratinized epithelial cells, a few polymorphonuclear neutrophils, and an occasional oddly shaped cell. Treatment consists of stopping the offending agent and using bland drops or none at all. Often the conjunctival reaction persists for weeks or months after its cause has been eliminated.
OCCUPATIONAL CONJUNCTIVITIS FROM CHEMICALS & IRRITANTS
Acids, alkalies, smoke, wind, and almost any irritating substance that enters the conjunctival sac may cause conjunctivitis. Some common irritants are fertilizers, soaps, deodorants, hair sprays, tobacco, makeup preparations (mascara, etc), and various acids and alkalies. In certain areas, smog has become the commonest cause of mild chemical conjunctivitis. The specific irritant in smog has not been positively identified, and treatment is nonspecific. There are no permanent ocular effects, but affected eyes are frequently chronically red and irritated.
In acid burns, the acids denature the tissue proteins and the effect is immediate. Alkalies do not denature the proteins but tend to penetrate the tissues deeply and rapidly and to linger in the conjunctival tissue. Here they continue to inflict damage for hours or days, depending on the molar concentration of the alkali and the amount introduced. Adhesion between the bulbar and palpebral conjunctiva (symblepharon) and corneal leukoma are more likely to occur if the offending agent is an alkali. In either event, pain, injection, photophobia, and blepharospasm are the principal symptoms of caustic burns. A history of the precipitating event can usually be elicited.
Immediate and profuse irrigation of the conjunctival sac with water or saline solution is of importance, and any solid material should be removed mechanically. Do not use chemical antidotes. Further treatment is with intensive topical steroids, ascorbate and citrate eyedrops, cycloplegics, antiglaucoma treatment as necessary, cold compresses, and systemic analgesics (see Chapter 19). Bacterial conjunctivitis may be treated with appropriate antibacterial agents. Corneal scarring may require corneal transplantation, and symblepharon may require a plastic operation on the conjunctiva. Severe conjunctival and corneal burns have a poor prognosis even with surgery, but if proper treatment is started immediately, scarring may be minimized and the prognosis improved.
CATERPILLAR HAIR CONJUNCTIVITIS (OPHTHALMIA NODOSUM)
On rare occasions, caterpillar hairs are introduced into the conjunctival sac, where they produce one or many granulomas (ophthalmia nodosum). Under magnification, each granuloma is seen to contain a small foreign body.
Treatment by removal of each hair individually is effective. If a hair is retained, invasion of the sclera and uveal tract may occur.
CONJUNCTIVITIS OF UNKNOWN CAUSE
FOLLICULOSIS
Folliculosis is a widespread benign, bilateral noninflammatory conjunctival condition characterized by follicular hypertrophy. It is more common in children than in adults, and the symptoms are minimal. The follicles are more numerous in the lower than in the upper cul-de-sac and tarsal conjunctiva. There is no associated inflammation or papillary hypertrophy, and complications do not occur.
There is no treatment for folliculosis, which disappears spontaneously after a course of 2-3 years. The cause is unknown, but folliculosis may be only a manifestation of a generalized adenoidal hypertrophy.
CHRONIC FOLLICULAR CONJUNCTIVITIS (Axenfeld's Conjunctivitis)
Chronic follicular conjunctivitis is a bilateral transmissible disease of children characterized by numerous follicles in the upper and lower tarsal conjunctiva. There are minimal conjunctival exudates and minimal inflammation but no complications. Treatment is ineffective, but the disease is self-limited within 2 years.
OCULAR ROSACEA
Ocular rosacea is a common complication of acne rosacea and probably occurs more often in light-skinned people, especially of Irish descent, than in dark-skinned people. It is usually a blepharoconjunctivitis, but the cornea is sometimes also affected. The patient complains of mild injection and irritation. There is frequently an accompanying staphylococcal blepharitis. The blood vessels of the lid margins are dilated and the conjunctiva hyperemic, especially in the exposed interpalpebral region. Less often, there may be a nodular conjunctivitis with small gray nodules on the bulbar conjunctiva, especially near the limbus, which may ulcerate superficially. The lesions can be differentiated from phlyctenules by the fact that even after they subside, the large dilated vessels persist.
Microscopic examination of the nodules shows lymphocytes and epithelial cells. The peripheral cornea may ulcerate and vascularize, and the keratitis may have a narrow base at the limbus and a wider infiltrate centrally. The corneal pannus is often segmented or wedge-shaped inferiorly (Figures 5-16 and 5-17).
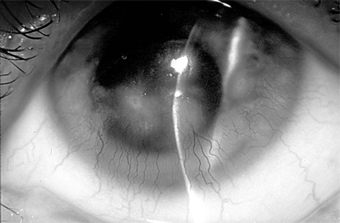
Figure 5-16: Chronic conjunctival injection and inferior keratopathy of rosacea. Note inferior pannus and corneal scarring suggestive of staphylococcal hypersensitivity.

Figure 5-17: Skin lesions in acne rosacea. (Courtesy of HB Ostler.)
Treatment of ocular rosacea consists of the elimination of hot, spicy foods and of alcoholic beverages that cause dilation of the facial vessels. Any secondary staphylococcal infection should be treated (Figure 5-18). A course of oral tetracycline or doxycycline is often helpful, and a smaller maintenance dose may be needed to control the disease.
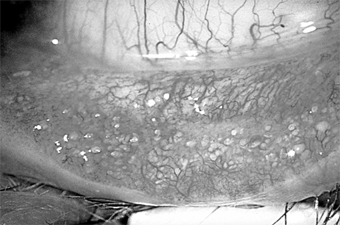
Figure 5-18: Multiple concretions on the inferior tarsus. These are often associated with chronic lid disease caused by staphylococcal species.
The disease is chronic, recurrences are common, and the response to treatment is usually poor. If the cornea is not affected, the visual prognosis is good; but corneal lesions tend to recur and progress, and the vision grows steadily worse over a period of years.
PSORIASIS
Psoriasis vulgaris usually affects the areas of the skin not exposed to the sun, but in about 10% of cases lesions appear on the skin of the eyelids, and the plaques may extend to the conjunctiva, where they cause irritation, a foreign body sensation, and tearing. Psoriasis can also cause nonspecific chronic conjunctivitis with considerable mucoid discharge. Rarely, the cornea may show marginal ulceration or a deep, vascularized opacity.
The conjunctival and corneal lesions wax and wane with the skin lesions and are not affected by specific treatment. In rare cases, conjunctival scarring (symblepharon, trichiasis), corneal scarring, and occlusion of the nasolacrimal duct have occurred.
ERYTHEMA MULTIFORME MAJOR (STEVENS-JOHNSON SYNDROME)
Erythema multiforme major is a disease of the mucous membranes and skin. The skin lesion is an erythematous, urticarial bullous eruption that appears suddenly and is often distributed symmetrically. Bilateral conjunctivitis, often membranous, is a common manifestation. The patient complains of pain, irritation, discharge, and photophobia. The cornea is affected secondarily, and vascularization and scarring may seriously reduce vision. Stevens-Johnson syndrome is typically a disease of young people, occurring only rarely after age 35.
Cultures are negative for bacteria; conjunctival scrapings show a preponderance of polymorphonuclear cells. Systemic steroids are thought to shorten the course of the systemic disease but have little or no effect on the eye lesions. Careful cleansing of the conjunctiva to remove the accumulated secretion is helpful, however, and tear replacement may be indicated. If trichiasis and entropion supervene, they should be corrected. Topical steroids probably have no beneficial effect, and their protracted use can cause corneal melting and perforation.
The acute episode of Stevens-Johnson syndrome usually lasts about 6 weeks, but the conjunctival scarring, loss of tears, and complications from entropion and trichiasis may result in prolonged morbidity and progressive corneal cicatrization. Recurrences are rare.
DERMATITIS HERPETIFORMIS
This is a rare skin disorder characterized by symmetrically grouped erythematous papulovesicular, vesicular, or bullous lesions. The disease has a predilection for the posterior axillary fold, the sacral region, the buttocks, and the forearms. Itching is often severe. Rarely, a pseudomembranous conjunctivitis occurs and may result in cicatrization resembling that seen in benign mucous membrane pemphigoid. The skin eruption and conjunctivitis usually respond readily to systemic sulfones or sulfapyridine.
EPIDERMOLYSIS BULLOSA
This is a rare hereditary disease characterized by vesicles, bullae, and epidermal cysts. The lesions occur chiefly on the extensor surfaces of the joints and other areas exposed to trauma. The severe dystrophic type that leads to scarring may also produce conjunctival scars similar to those seen in dermatitis herpetiformis and benign mucous membrane pemphigoid. No known treatment is satisfactory.
SUPERIOR LIMBIC KERATOCONJUNCTIVITIS
Superior limbic keratoconjunctivitis is usually bilateral and limited to the upper tarsus and upper limbus. The principal complaints are irritation and hyperemia. The signs are papillary hypertrophy of the upper tarsus, redness of the superior bulbar conjunctiva, thickening and keratinization of the superior limbus, epithelial keratitis, recurrent superior filaments, and superior micropannus (Figure 5-19). Rose bengal staining is a helpful diagnostic test. The keratinized epithelial cells and mucous debris pick up the stain. Scrapings from the upper limbus show keratinizing epithelial cells.
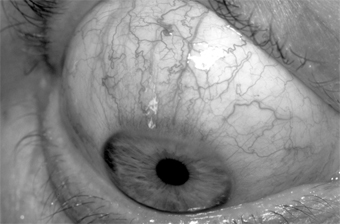
Figure 5-19: Superior limbic keratoconjunctivitis. Note the "corridor" on the bulbar surface.
In about 50% of cases, the condition has been associated with abnormal function of the thyroid gland. Applying 0.5% or 1% silver nitrate to the upper palpebral conjunctiva and allowing the tarsus to drop back onto the upper limbus usually result in shedding of the keratinizing cells and relief of symptoms for 4-6 weeks. This treatment can be repeated. There are no complications, and the disease usually runs a course of 2-4 years.
In severe cases, one may consider 5 mm resection of the perilimbal superior conjunctiva.
LIGNEOUS CONJUNCTIVITIS
This is a rare bilateral, chronic or recurrent, pseudomembranous or membranous conjunctivitis that arises early in life, predominantly in young girls, and often persists for many years. Granulomas are often associated with it, and the lids may feel very hard. Cyclosporine may be effective treatment, as suggested by recent reports.
REITER'S SYNDROME
A triad of disease manifestations-nonspecific urethritis, arthritis, and conjunctivitis or iritis-constitutes Reiter's syndrome. The disease occurs much more often in men than in women. The conjunctivitis is papillary in type and usually bilateral. Conjunctival scrapings contain polymorphonuclear cells. No bacteria grow in cultures. The arthritis usually affects the large weight-bearing joints. There is no satisfactory treatment, though nonsteroidal anti-inflammatory agents may be effective. Corticosteroids will help the iridocyclitis. The disease has been found in association with HLA-B27 antigen.
MUCOCUTANEOUS LYMPH NODE SYNDROME (KAWASAKI DISEASE)
This disease of unknown cause was first described in Japan in 1967. Conjunctivitis is one of its six diagnostic features. The others are (1) fever that fails to respond to antibiotics; (2) changes in the lips and oral cavity; (3) such changes in the extremities as erythema of the palms and soles, indurative edema, and membranous desquamation of the fingertips; (4) polymorphous exanthem of the trunk; and (5) acute nonpurulent swelling of the cervical lymph nodes.
The disease occurs almost exclusively in prepubertal children and carries a 1-2% mortality rate from cardiac failure. The conjunctivitis has not been severe, and no corneal lesions have been reported.
Treatment is supportive only.
CONJUNCTIVITIS ASSOCIATED WITH SYSTEMIC DISEASE
CONJUNCTIVITIS IN THYROID DISEASE
In orbital Graves' disease, the conjunctiva may be red and chemotic and the patient may complain of copious tearing. As the disease progresses, the chemosis increases, and in advanced cases the chemotic conjunctiva may extrude between the lids (Figure 5-20).
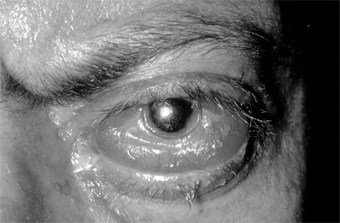
Figure 5-20: Graves' disease. Note conjunctival prolapse, keratinization, and marked chemosis and injection.
Treatment is directed toward control of the thyroid disease, and every effort must be made to protect the conjunctiva and cornea by bland ointment, surgical lid adhesions (tarsorrhaphy) if necessary, or even orbital decompression if the lids do not close enough to cover the cornea and conjunctiva.
GOUTY CONJUNCTIVITIS
Patients with gout often complain of a "hot eye" during attacks. On examination, a mild conjunctivitis is found that is less severe than suggested by the symptoms. Gout may also be associated with episcleritis or scleritis, iridocyclitis, keratitis, vitreous opacities, and retinopathy. Treatment is aimed at controlling the gouty attack with colchicine and allopurinol.
CARCINOID CONJUNCTIVITIS
In carcinoid, the conjunctiva is sometimes congested and cyanotic as a result of the secretion of serotonin by the chromaffin cells of the gastrointestinal tract. The patient may complain of a "hot eye" during such attacks.
CONJUNCTIVITIS SECONDARY TO DACRYOCYSTITIS OR CANALICULITIS
CONJUNCTIVITIS SECONDARY TO DACRYOCYSTITIS
Both pneumococcal conjunctivitis (often unilateral and unresponsive to treatment) and beta-hemolytic streptococcal conjunctivitis (often hyperacute and purulent) may be secondary to chronic dacryocystitis. The nature and source of the conjunctivitis in both instances are often missed until the lacrimal system is investigated.
CONJUNCTIVITIS SECONDARY TO CANALICULITIS
Canaliculitis due to canalicular infection with Actinomyces israelii or Candida species (or, very rarely, Aspergillus species) may cause unilateral mucopurulent conjunctivitis, often chronic. The source of the condition is often missed unless the characteristic hyperemic, pouting punctum is noted. Expression of the canaliculus (upper or lower, whichever is involved) is curative provided the entire concretion is removed.
Conjunctival scrapings show a predominance of polymorphonuclear cells. Cultures (unless anaerobic) are usually negative. Candida grows readily on ordinary culture media, but almost all of the infections are caused by A israelii, which requires an anaerobic medium.
II. DEGENERATIVE DISEASES OF THE CONJUNCTIVA
PINGUECULA
Pingueculae are extremely common in adults. They appear as yellow nodules on both sides of the cornea (more commonly on the nasal side) in the area of the palpebral aperture. The nodules, consisting of hyaline and yellow elastic tissue, rarely increase in size, but inflammation is common. In general, no treatment is required, but in certain cases of pingueculitis, weak topical steroids (eg, prednisolone 0.12%) or topical nonsteroidal anti-inflammatory medications may be given (Figure 5-21).

Figure 5-21: Pinguecula. (Courtesy of A Rosenberg.)
PTERYGIUM
A pterygium is a fleshy, triangular encroachment of a pinguecula onto the cornea, usually on the nasal side bilaterally (Figure 5-22). It is thought to be an irritative phenomenon due to ultraviolet light, drying, and windy environments, since it is common in persons who spend much of their lives out of doors in sunny, dusty, or sandy, windblown surroundings. The pathologic findings in the conjunctiva are the same as those of pinguecula. In the cornea, there is replacement of Bowman's layer by hyaline and elastic tissue.

Figure 5-22: Pterygium encroaching on the cornea.
If the pterygium is enlarging and encroaches on the pupillary area, it should be removed surgically along with a small portion of superficial clear cornea beyond the area of encroachment. Beta-irradiation, topical mitomycin C, and conjunctival autografting have all been used to reduce the risk of recurrent disease.
CLIMATIC DROPLET KERATOPATHY (BIETTI'S BAND-SHAPED NODULAR DYSTROPHY, LABRADOR KERATOPATHY, SPHEROIDAL DEGENERATION)
Climatic droplet keratopathy is an uncommon degenerative disorder of the cornea characterized by aggregates of yellowish-golden spherules that accumulate in the subepithelial layers. The cause is unknown, but certain factors such as exposure to ultraviolet light, aridity, and microtrauma are recognized predisposing factors. The deposits may result in elevation of the epithelium in a band-shaped configuration. The condition is more common in geographic regions with high levels of direct and reflected sunlight.
III. MISCELLANEOUS DISORDERS OF THE CONJUNCTIVA
LYMPHANGIECTASIS
Lymphangiectasis is characterized by localized small, clear, tortuous dilations in the conjunctiva. They are merely dilated lymph vessels, and no treatment is indicated unless they are irritating or cosmetically objectionable. They can then be cauterized or excised (Figure 5-23).
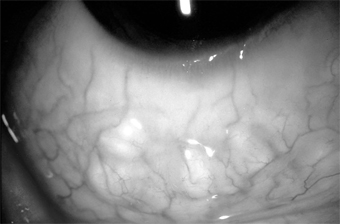
Figure 5-23: Conjunctival lymphangiectasis. Note the clear tortuous dilations in the conjunctiva.
CONGENITAL CONJUNCTIVAL LYMPHEDEMA
This is a rare entity, unilateral or bilateral, and characterized by pinkish, fleshy edema of the bulbar conjunctiva. Usually observed as an isolated entity at birth, the condition is thought to be due to a congenital defect in the lymphatic drainage of the conjunctiva. It has been observed in chronic hereditary lymphedema of the lower extremities (Milroy's disease) and is thought to be an ocular manifestation of this disease rather than an associated anomaly.
CYSTINOSIS
Cystinosis is a rare congenital disorder of amino acid metabolism characterized by widespread intracellular deposition of cystine crystals in various body tissues, including the conjunctiva and cornea. Three types are recognized: childhood, adolescent, and adult. Life expectancy is reduced in the first two types.
SUBCONJUNCTIVAL HEMORRHAGE
This common disorder may occur spontaneously, usually in only one eye, in any age group. Its sudden onset and bright red appearance usually alarm the patient. The hemorrhage is caused by rupture of a small conjunctival vessel, sometimes preceded by a bout of severe coughing or sneezing (Figure 5-24).
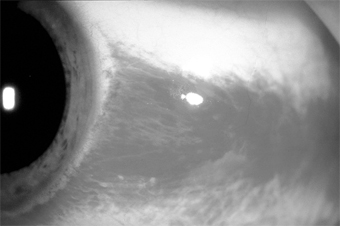
Figure 5-24: Subconjunctival hemorrhage.
The best treatment is reassurance. The hemorrhage usually absorbs in 2-3 weeks.
In rare instances the hemorrhages are bilateral or recurrent; the possibility of blood dyscrasias should then be ruled out.
OPHTHALMIA NEONATORUM
Ophthalmia neonatorum in its broad sense refers to any infection of the newborn conjunctiva. In its narrow and commonly used sense, however, it refers to a conjunctival infection, chiefly gonococcal, that follows contamination of the baby's eyes during its passage through the mother's cervix and vagina or during the postpartum period. Because gonococcal conjunctivitis can rapidly cause blindness, the cause of all cases of ophthalmia neonatorum should be verified by examination of smears of exudate, epithelial scrapings, cultures, and rapid tests for gonococci.
Gonococcal neonatal conjunctivitis causes corneal ulceration and blindness if not treated immediately. Chlamydial neonatal conjunctivitis (inclusion blennorrhea) is less destructive but can last months if untreated and may be followed by pneumonia. Other causes include infections with staphylococci, pneumococci, Haemophilus, and herpes simplex virus and silver nitrate prophylaxis.
The time of onset is important but not entirely reliable in clinical diagnosis since the two principal types, gonorrheal ophthalmia and inclusion blennorrhea, have widely differing incubation periods: gonococcal disease 2-3 days and chlamydial disease 5-12 days. The third important birth canal infection (HSV-2 keratoconjunctivitis) has a 2- to 3-day incubation period and is potentially quite serious because of the possibility of systemic dissemination.
Treatment for neonatal gonococcal conjunctivitis is with ceftriaxone, 125 mg as a single intramuscular dose; a second choice is kanamycin, 75 mg intramuscularly. To treat chlamydial conjunctivitis in newborns, erythromycin oral suspension is effective at a dosage of 40 mg/kg/d in four divided doses for 2 weeks. In both gonococcal and chlamydial conjunctivitis, the parents need to be treated. Herpes simplex keratoconjunctivitis is treated with acyclovir, 30 mg/kg/d in three divided doses for 14 days. Neonatal disease from HSV requires hospitalization because of the potential neurologic or systemic manifestations. Other types of neonatal conjunctivitis are treated with erythromycin, gentamicin, or tobramycin ophthalmic ointment four times daily.
Credé 1% silver nitrate prophylaxis is effective for the prevention of gonorrheal ophthalmia but not inclusion blennorrhea or herpetic infection. The slight chemical conjunctivitis induced by silver nitrate is minor and of short duration. Accidents with concentrated solutions can be avoided by using wax ampules specially prepared for Credé prophylaxis. Tetracycline and erythromycin ointment are effective substitutes.
OCULOGLANDULAR DISEASE (PARINAUD'S OCULOGLANDULAR SYNDROME)
This is a group of conjunctival diseases, usually unilateral, characterized by low-grade fever, grossly visible preauricular adenopathy, and one or more conjunctival granulomas (Figure 5-25). The commonest cause is cat-scratch disease, but there are many other causes, including Mycobacterium tuberculosis, Treponema pallidum, Francisella tularensis, Pasteurella (Yersinia) pseudotuberculosis, Chlamydia trachomatis serotypes L1, L2, and L3, and Coccidioides immitis.

Figure 5-25: Conjunctival granuloma. (Courtesy of P Thygeson.)
Conjunctival Cat-Scratch Disease
This protracted but benign granulomatous conjunctivitis is found most commonly in children who have been in intimate contact with cats. The child often runs a low-grade fever and develops a reasonably enlarged preauricular node and one or more conjunctival granulomas. These may show focal necrosis and may sometimes ulcerate. The regional adenopathy does not suppurate. The clinical diagnosis is supported by serology.
The disease appears to be caused by a slender pleomorphic gram-negative bacillus (Bartonella [formerly Rochalimaea] henselae), which grows in the walls of blood vessels. With special stains, this organism can be seen in biopsies of conjunctival tissue. The organism closely resembles Leptotrichia buccalis, and the disease was previously known as leptotrichosis conjunctivae (Parinaud's conjunctivitis). The organism is commonly found in the mouth in humans and always in the mouth in cats. The eye may be contaminated by saliva on the child's fingers or by cat saliva on the child's pillow. Afipia felis has been incriminated also and may still play a role.
The disease is self-limited (without corneal or other complications) and resolves in 2-3 months. The conjunctival nodule can be excised; in the case of a solitary granuloma, this may be curative. Systemic tetracyclines may shorten the course but should not be given to children under 7 years of age.
Conjunctivitis Secondary to Neoplasms (Masquerade Syndrome)
When examined superficially, a neoplasm of the conjunctiva or lid margin is often misdiagnosed as a chronic infectious conjunctivitis or keratoconjunctivitis. Since the underlying lesion is often not recognized, the condition has been referred to as masquerade syndrome. The masquerading neoplasms on record are conjunctival capillary carcinoma, conjunctival carcinoma in situ, infectious papilloma of the conjunctiva, sebaceous gland carcinoma, and verrucae. Verrucae and molluscum tumors of the lid margin may desquamate toxic tumor material that produces a chronic conjunctivitis, keratoconjunctivitis, or (rarely) keratitis alone.
IV. CONJUNCTIVAL TUMORS
PRIMARY BENIGN TUMORS OF THE CONJUNCTIVA
Nevus (Figure 5-26)
One-third of melanocytic nevi of the conjunctiva lack pigment. Over half have cystic epithelial inclusions that can be seen clinically.
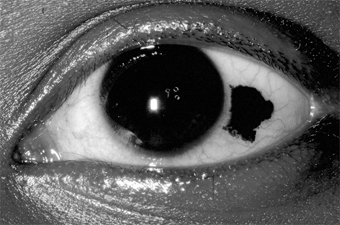
Figure 5-26: Conjunctival nevus. Note sharp borders.
Histologically, conjunctival nevi are composed of nests or sheets of nevus cells. Conjunctival nevi, like other nevi, rarely become malignant. Many are excised because they are disfiguring.
Pigmented conjunctival nevi must be distinguished from primary acquired melanosis of the conjunctiva. The latter occurs later in life (after the third decade), is usually unilateral, tends to wax and wane in degree of pigmentation, and, depending on the degree of cellular atypia, has a risk of becoming malignant ranging from nil to 90%.
Papilloma
Conjunctival papillomas occur in two forms: infectious papillomas, associated with a papovavirus, occurs in children and young adults, especially in the inferior fornix and near the medial canthus (Figure 5-27). The other type arises from a broad base, often near the limbus, in older adults and may be indistinguishable from conjunctival intraepithelial neoplasia. A biopsy may be required to establish the diagnosis.

Figure 5-27: Conjunctival papilloma.
Granulomatous Inflammation
Granulomatous inflammation occurs around foreign bodies, around extravasated sebaceous material in chalazia, and in association with diseases such as coccidioidomycosis and sarcoidosis. These inflammatory foci may form elevated plaques or nodules in the skin or the conjunctiva of the eyelids.
Dermoid Tumor (Figure 5-28)
This congenital tumor appears as a smooth, rounded, yellow elevated mass, frequently with hairs protruding. A dermoid tumor may remain quiescent, though it can increase in size. Removal is indicated only if cosmetic deformity is significant or if vision is impaired or threatened. Limbal dermoids and dermolipomas are most often isolated lesions, but occasionally they may be part of such syndromes as oculoauriculovertebral dysplasia (Goldenhar's syndrome).
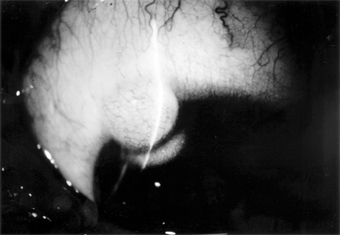
Figure 5-28: Conjunctival dermoid tumor.
Dermolipoma
Dermolipoma is a common congenital tumor that usually appears as a smoothly rounded growth in the upper temporal quadrant of the bulbar conjunctiva near the lateral canthus. Treatment is usually not indicated, but at least partial removal may be indicated if the growth is enlarging or is cosmetically disfiguring. Posterior dissection must be undertaken with extreme care (if at all) since this lesion is frequently continuous with orbital fat; orbital derangement may cause scarring and complications far more serious than the original lesion.
Lymphoma & Lymphoid Hyperplasia
These are conjunctival lesions that may appear in adults without evidence of systemic disease or associated with systemic lymphosarcoma or various blood dyscrasias. The clinical appearance of benign lymphoid hyperplasia and malignant lymphoma can be similar; therefore, biopsy is essential to establish a diagnosis. Since many of these lymphoid tumors may involve the orbit, an magnetic resonance imaging (MRI) or computed tomography (CT) scan may be required to determine the true extent of the tumor.
Treatment of both benign and malignant lesions is best accomplished with radiotherapy.
Angioma
Conjunctival angiomas may occur as isolated, circumscribed capillary hemangiomas or as more diffuse vascular tumors, often associated with a more extensive lid or orbital capillary or cavernous hemangioma. Hemangiomas should be distinguished from telangiectases involving conjunctival capillaries. Telangiectatic conjunctival vessels may occur as isolated lesions or may be associated with systemic vascular hamartomas in Rendu-Osler-Weber disease or in ataxia-telangiectasia (Louis-Bar syndrome).
Pyogenic granulomas are a variety of capillary hemangiomas. They frequently occur on the palpebral conjunctiva over chalazia or in an area of recent surgery.
In Kaposi's sarcoma associated with AIDS, red-blue vascular nodules may first become apparent in the conjunctiva. They are associated with a herpesvirus. Radiotherapy is the most effective treatment.
Bacillary angiomatosis is another proliferative vascular lesion that may appear similar to Kaposi's sarcoma. It is due to infection with gram-negative bacteria of the genus Bartonella-B henselae from cats in patients with AIDS and B quintana from body lice in low-income homeless individuals. These tumors respond to antibiotic therapy.
PRIMARY MALIGNANT TUMORS OF THE BULBAR CONJUNCTIVA
Carcinoma
Carcinoma of the conjunctiva arises most frequently at the limbus in the area of the palpebral fissure and less often in nonexposed areas of the conjunctiva. Some of these tumors may resemble pterygia. Most have a gelatinous surface; sometimes, abnormal keratinization of the epithelium produces leukoplakia. Growth is slow, and deep invasion and metastases are extremely rare; therefore, complete excision is effective treatment. Recurrences are common if the lesion is incompletely excised; treatment consists of reexcision. The use of cryotherapy may help to prevent recurrences.
Conjunctival dysplasia, also called atypical epithelial dysplasia, is a benign condition that occurs as an isolated lesion or sometimes over pterygia and pingueculae and can resemble carcinoma in situ clinically and even histologically. The term conjunctival intraepithelial neoplasia can be applied to all neoplastic lesions from dysplasia to carcinoma that are confined to the epithelium.
Excisional biopsy will establish a diagnosis and result in cure of most of these lesions.
Malignant Melanoma
Malignant melanomas of the conjunctiva are rare. Most arise from areas of primary acquired melanosis; some arise from conjunctival nevi; a few apparently arise de novo from normal conjunctiva. Some are melanotic; others are heavily pigmented (Figure 5-29).
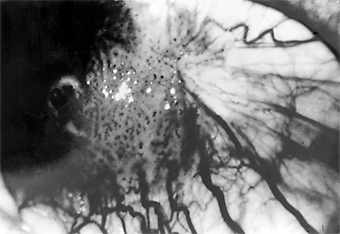
Figure 5-29: Conjunctival malignant melanoma.
Many tumors can be locally excised. More radical surgery (eg, exenteration of the orbit) does not usually improve the prognosis. The use of cryotherapy after excision of melanotic tumors may help to prevent recurrences.
REFERENCESList of Figures
| Figure 5-1: Gonococcal conjunctivitis. Profuse purulent exudate. (Courtesy of L Schwab.) | |
| Figure 5-2: Advanced trachoma following corneal ulceration and scarring. Note the fly on the temporal aspect of the lower lid. The fly is a principal vector for trachoma. | |
| Figure 5-3: Acute follicular conjunctivitis caused by inclusion conjunctivitis in a 22-year-old man with urethritis. (Courtesy of K Tabbara.) | |
| Figure 5-4: Acute follicular conjunctivitis due to adenovirus type 3. (Courtesy of P Thygeson.) | |
| Figure 5-5: Epidemic keratoconjunctivitis. Thick white membrane of upper palpebral conjunctiva. | |
| Figure 5-6: Mononuclear cell reaction in conjunctival scrapings of a patient with viral conjunctivitis caused by adenovirus type 8. (Courtesy of M Okumoto.) | |
| Figure 5-7: Primary ocular herpes. (Courtesy of HB Ostler.) | |
| Figure 5-8: Acute hemorrhagic conjunctivitis. | |
| Figure 5-9: Molluscum contagiosum of lid margin. Follicular conjunctivitis was present. | |
| Figure 5-10: Acute hypersensitivity with moderate tylosis, moderate to marked chemosis and mild injection of the conjunctiva. Note that the eye seems to be "sinking" into the surrounding tissue. | |
| Figure 5-11: Vernal keratoconjunctivitis. "Cobblestone" papillae on superior tarsal conjunctiva. | |
| Figure 5-12: Moderate to marked papillary response of upper tarsus seen in atopic keratoconjunctivitis. | |
| Figure 5-13: Phlyctenulosis. Note three phlyctenules along the inferior limbus, each with an umbilicated center. | |
| Figure 5-14: Contact dermatitis secondary to neomycin. Note lower lid involvement. | |
| Figure 5-15: Mononuclear infiltration of the accessory salivary glands of a patient with Sjögren's syndrome. (Courtesy of K Tabbara.) | |
| Figure 5-16: Chronic conjunctival injection and inferior keratopathy of rosacea. Note inferior pannus and corneal scarring suggestive of staphylococcal hypersensitivity. | |
| Figure 5-17: Skin lesions in acne rosacea. (Courtesy of HB Ostler.) | |
| Figure 5-18: Multiple concretions on the inferior tarsus. These are often associated with chronic lid disease caused by staphylococcal species. | |
| Figure 5-19: Superior limbic keratoconjunctivitis. Note the "corridor" on the bulbar surface. | |
| Figure 5-20: Graves' disease. Note conjunctival prolapse, keratinization, and marked chemosis and injection. | |
| Figure 5-21: Pinguecula. (Courtesy of A Rosenberg.) | |
| Figure 5-22: Pterygium encroaching on the cornea. | |
| Figure 5-23: Conjunctival lymphangiectasis. Note the clear tortuous dilations in the conjunctiva. | |
| Figure 5-24: Subconjunctival hemorrhage. | |
| Figure 5-25: Conjunctival granuloma. (Courtesy of P Thygeson.) | |
| Figure 5-26: Conjunctival nevus. Note sharp borders. | |
| Figure 5-27: Conjunctival papilloma. | |
| Figure 5-28: Conjunctival dermoid tumor. | |
| Figure 5-29: Conjunctival malignant melanoma. |
List of Tables
| Table 5-1: Causes of conjunctivitis. | |
| Table 5-2: Differentiation of the common types of conjunctivitis. |
10.1036/1535-8860.ch5